Circ Res:Dynamin相关蛋白1抑制可以减轻氧化应激下心血管的钙化
2017-06-18 MedSci MedSci原创
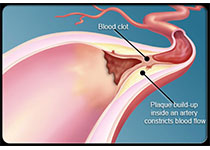
细胞的分化和心血管疾病过程中伴随着线粒体的变化。动力蛋白相关蛋白1(DRP1)是线粒体分裂的关键调节剂。近期,一项发表在杂志Circ Res上的研究评估了DRP1在心血管钙化中的作用。探讨了成骨促进条件对DRP1的影响,以及DRP1抑制剂是否改变心血管钙化的发展。此项研究采用免疫组织化学检测,发现DRP1富集于人颈动脉钙化区。原代血管平滑肌细胞(SMC)的成骨分化增加了DRP1表达。人SMC在成骨
细胞的分化和心血管疾病过程中伴随着线粒体的变化。动力蛋白相关蛋白1(DRP1)是线粒体分裂的关键调节剂。
此项研究采用免疫组织化学检测,发现DRP1富集于人颈动脉钙化区。原代血管平滑肌细胞(SMC)的成骨分化增加了DRP1表达。人SMC在成骨分化过程中,DRP1抑制剂减弱了基质矿化,细胞骨架重排,线粒体功能障碍,同时减少了1型胶原的分泌和碱性磷酸酶活性。
在钙化的人主动脉瓣中也观察到了DRP1蛋白,并且DRP1 RNA干扰降低了原代人类瓣膜间质细胞的钙化。
在PCSK9获得功能动脉粥样硬化模型中,Drp1缺失的杂合小鼠并未表现出血管病变。然而,当通过氧化应激诱导矿化时,DRP1抑制剂减弱了小鼠和人类SMC的钙化。对于Drp1的缺失,小鼠的股骨骨密度不变,DRP1抑制剂减弱了人类骨成骨细胞的氧化应激介导的功能障碍。
此项研究表明了DRP1在调节胶原分泌和心血管钙化方面的新功能,这是探索新的治疗心血管疾病细胞纤维化反应的新疗法的一个探索领域。此外,此项研究还支持了线粒体动力学在调节氧化应激介导的动脉钙应激和骨丢失中的作用。
原始出处:
Rogers M, Maldonado-Martinez N, et al. Dynamin-Related Protein 1 Inhibition Attenuates Cardiovascular Calcification in the Presence of Oxidative Stress. Circ Res. 2017 Jun 12. pii: CIRCRESAHA.116.310293. doi: 10.1161/CIRCRESAHA.116.310293.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#应激#
30
学习了受益匪浅学习
60
学习了分享了
62