Thorac Cancer:伴有EGFR-T790M突变的NSCLC患者,后续奥希替尼不同顺序治疗生存对比
2021-11-24 yd2015 MedSci原创
研究表明,1/2代EGFR-TKI治疗进展后出现T790M突变患者,化疗可影响后续奥希替尼治疗的疗效。
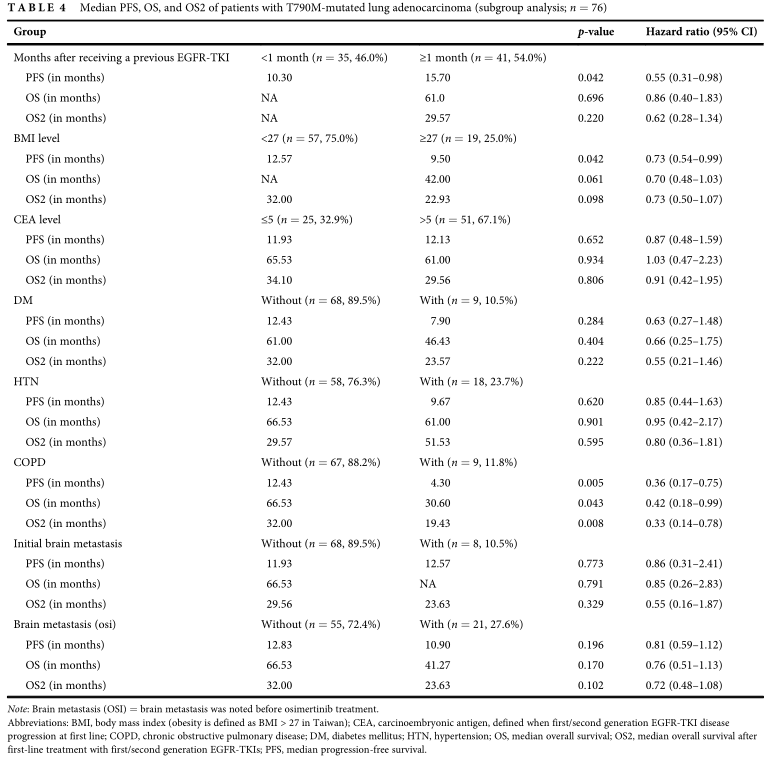
目前晚期NSCLC患者伴有EGFR-T790M突变时,标准治疗为第三代EGFR-TKI奥希替尼。而对于第一代/第二代表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKIs)治疗后获得T790M突变患者,后续奥希替尼不同顺序治疗的获益情况尚不明确。因此来自我国台湾的团队开展了相关研究,相关结果发表在Thoracic Cancer杂志上。
研究回顾性筛选2013至2019年间在高雄长庚纪念医院诊断为癌症的3807例患者。共有76例EGFR-T790M突变患者在重新活检或液体活检后接受奥希替尼被纳入分析。分为两组:A组为患者接受奥希替尼前接受化疗(n=36);B组为1/2代EGFR-TKI治疗进展后直接奥希替尼治疗(n=40)。36例患者中,35例(97.2%)患者接受顺铂/卡铂联合培美曲塞治疗,1例(2.8%)患者接受卡铂联合多西他赛。在这36名患者中,没有一名接受抗血管生成治疗。平均年龄61.91±10.49(范围:36-81)年(A组:62.61±9.82组,B组61.28±11.15);男性30例(39.5%),女性46例(60.5%)(A组:12/24 [33.3%/66.7%],B组:18/22[45.0%/55.0%])。
初诊时EGFR基因分型显示42例(55.3%)和34例(44.7%)腺癌患者中分别存在Del 19和L858R突变。所有患者均接受EGFR-TKIs治疗:36例(47.4%),21例(27.6%),19例(25.0%)分别接受吉非替尼、厄洛替尼和阿法替尼。进展后再次活检或血液检查提示42例患者Del 19突变伴有T790M突变(55.3%)和34例患者L858R突变伴有T790M突变。
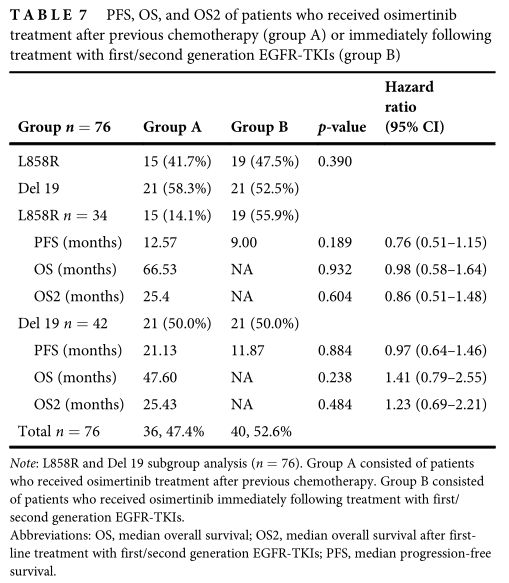
76例患者中,40例(52.6%)、25例(32.9%)和11例(14.5%)分别达到部分缓解、病情稳定和疾病进展。ORR为52.6%,DCR为85.5%。此外,他们的中位PFS、中位OS和中位OS2分别为11.93、66.53和29.57个月。
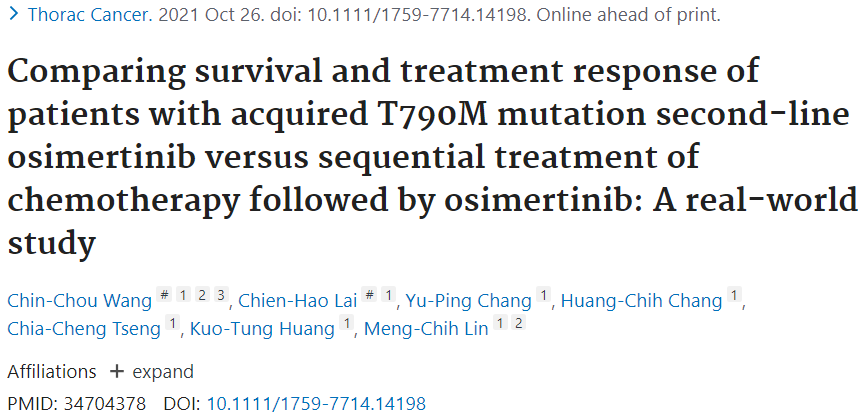
吉非替尼、阿法替尼或厄洛替尼一线治疗后接受奥希替尼治疗的患者中位PFS分别为12.83个月、11.93个月和10.9个月(p = 0.424)。吉非替尼、阿法替尼、厄洛替尼一线治疗后接受奥希替尼治疗的患者中位OS分别为87.93、49.00和42个月;此外,一线使用不同EGFR-TKIs治疗的患者的OS无显著差异(p = 0.484),但吉非替尼组的OS似乎更长(87.93个月)。使用吉非替尼、阿法替尼或厄洛替尼一线治疗后接受奥希替尼治疗的患者中位OS2分别为22.73、16.1和34个月。
A、B两组在ORR方面无差异(63.9% vs 42.5%,p = 0.063),但DCR有差异(94.4% vs 77.5%,p = 0.036)。两组间PFS(15.7个月vs. 10.83个月,p = 0.248)、OS(49.00个月vs. NA, p = 0.430)、OS2(25.43个月vs. NA, p = 0.933)无显著差异。

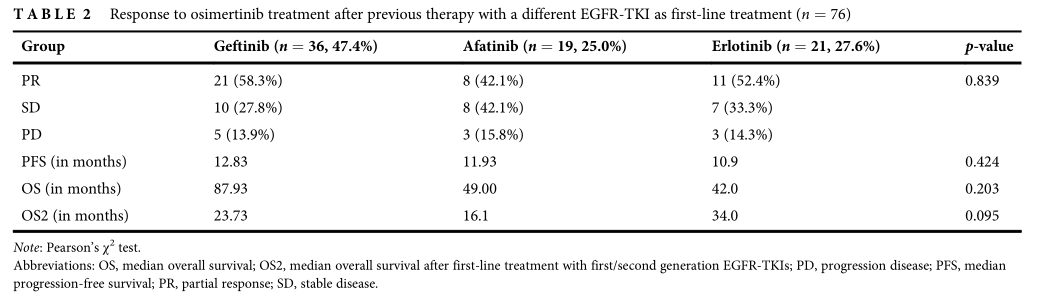
亚组分析显示,对于PFS,以下因素观察到显著差异:患者接受EGFR-TKI治疗≥1个月(p = 0.042,HR= 0.55, 95%CI = 0.31 - 0.98),低BMI (p = 0.042, HR = 0.73, 95% CI 0.99 = 0.54),没有慢性阻塞性肺疾病(COPD) (p = 0.005,HR= 0.36, 95%CI = 0.17-0.75)。OS仅在无COPD患者中有显著差异(p = 0.043, HR = 0.42, 95% CI = 0.18-0.99)。OS2仅在无COPD患者中有显著差异(p = 0.008, HR = 0.33, 95% CI = 0.14-0.78)。多因素分析,CPOD是PFS和OS2的不良因素。

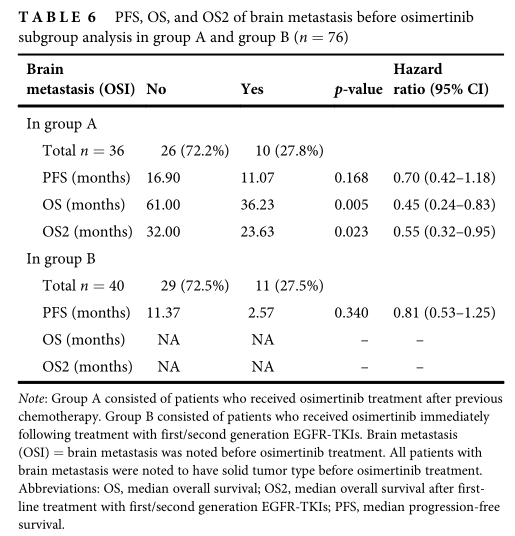
A组有10例(27.8%)患者在使用奥希替尼前发生脑转移;奥希替尼治疗前发生脑转移的患者PFS为11.07个月,未发生脑转移的患者PFS为16.90个月。B组11例(27.5%)患者在使用奥希替尼前发生脑转移;奥希替尼治疗前发生脑转移的患者PFS为10.27个月,未发生脑转移的患者PFS为11.37个月。因此,奥西替尼作为三线治疗的PFS优于二线治疗。
研究者还研究了L858R与Del19突变患者的生存率差异。L858R阳性患者中,A组和B组PFS无显著差异(12.57个月vs. 9.00个月,p = 0.189)。此外,在del19阳性患者中,A组和B组PFS无显著差异(21.13个月vs. 11.87个月,p = 0.884)。然而,A组L858R和del19阳性患者的PFS较长。
综上,研究表明,1/2代EGFR-TKI治疗进展后出现T790M突变患者,化疗可影响后续奥希替尼治疗的疗效。
原始出处:
Wang CC, Lai CH, Chang YP, Chang HC, Tseng CC, Huang KT, Lin MC. Comparing survival and treatment response of patients with acquired T790M mutation second-line osimertinib versus sequential treatment of chemotherapy followed by osimertinib: A real-world study. Thorac Cancer. 2021 Oct 26. doi: 10.1111/1759-7714.14198. Epub ahead of print. PMID: 34704378.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SCLC患者#
58
#T790M#
33
#THORAC#
33
#NSCLC患者#
37
#GFR#
37