J Thorac Onco:奥希替尼单药抗NSCLC患者未放疗过的CNS转移灶的疗效
2021-08-26 Nebula MedSci原创
奥斯替尼单药在携带EGFR激活突变的非小细胞肺癌患者中具有抗中枢神经系统转移的疗效
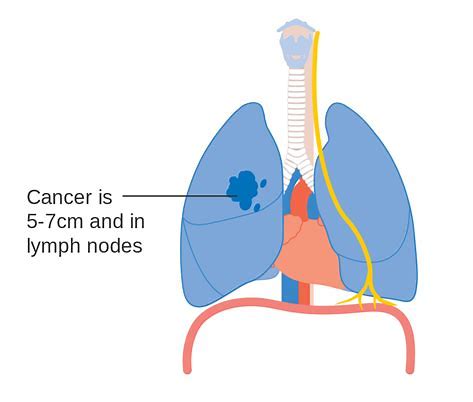
奥希替尼(Osimertinib)已被报道可有效治疗表皮生长因子受体(EGFR)激活性突变阳性的非小细胞肺癌(NSCLC)患者的中枢神经系统(CNS)转移灶。但是,由于既往相关研究纳入的病例都是接受过放疗的,可能存在放疗后肿瘤缩小延迟的效益,因此单用奥希替尼治疗CNS转移的真实抗肿瘤活性仍不能完全明确。
OCEAN研究旨在评估奥希替尼抗EGFR敏感性突变阳性的NSCLC患者的未放疗过的CNS转移灶的疗效。
该研究包含两个队列试验,共招募了66位符合要求的患者(T790M队列,n=40;一线队列,n=26)。受试患者每日接受80 mg的奥希替尼治疗。主要终点是根据PAREXEL标准的脑转移缓解率(BMRR)。本文报告了T790M队列的研究结果,包括药物浓度和血浆ctDNA分析结果。
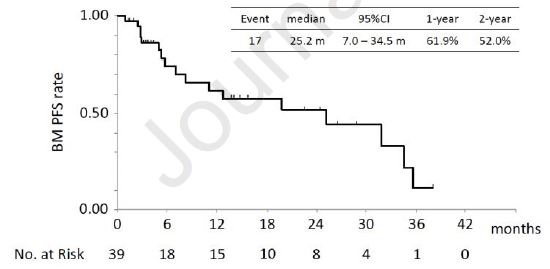
39位患者的脑转移无进展生存期
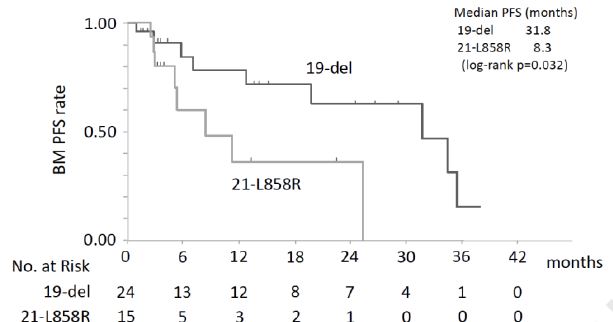
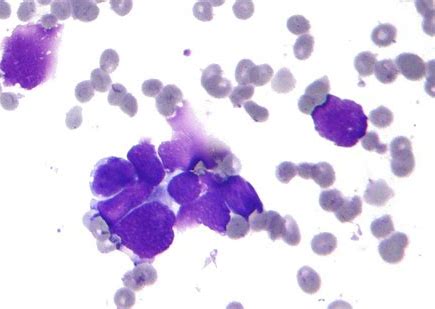
患者中位年龄为69岁,30%的男性。8位(20%)患者有CNS转移症状,大部分为多发性CNS转移(78%)。在39位可评估的患者中,中位脑转移相关的无进展生存期(PFS)、中位总生存期(OS)、总缓解率和中位PFS分别是66.7%(95% CI 54.3-79.1%)、25.2个月、19.8个月、40.5%和7.1个月。EGFR第19外显子缺失的患者的脑转移相关PFS明显长于EGFR第21外显子L858R的患者(中位值:31.8 vs 8.3;p=0.032)。
根据EGFR突变分组的脑转移PFS
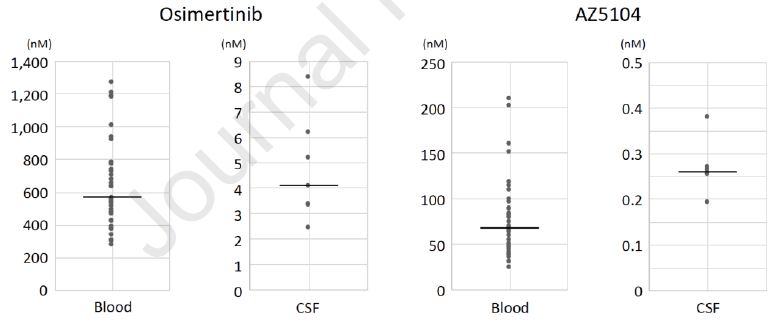
在第22天及以后,奥希替尼的血液低谷和脑脊液(CSF)中位浓度分别是569 nM和4.10 nM,而AZ5104对应的两处的浓度分别是68.0 nM和0.260 nM。奥斯替尼和AZ5104的血液与CSF中位浓度比值分别是0.79%和0.53%。第22天时的血液低谷浓度与奥斯替尼抗CNS转移的疗效无相关性。
奥斯替尼和AZ5104的血液与CSF浓度
治疗前,分别在83%和3%的患者的血浆中检测到了T790M和C797S突变;在第22天时,T790M和C797S突变的检出率分别是11%和3%;在检测到病情进展时,两个突变的检出率分别是39%和22%。
总之,该研究评估了奥希替尼抗EGFR T790M阳性NSCLC患者未放疗过的CNS转移的疗效。主要终点达标,研究结果证实了奥希替尼在携带EGFR T790M突变的患者的CNS转移的效果,特别是在携带EGFR 第19外显子缺失的患者中。
原始出处:
Yamaguchi Hiroyuki,Wakuda Kazushige,Fukuda Minoru et al. A phase II study of osimertinib for radiotherapy-na?ve CNS metastasis from non-small cell lung cancer: Results for the T790M cohort of the OCEAN study (LOGIK1603/WJOG9116L). J Thorac Oncol, 2021, https://doi.org/10.1016/j.jtho.2021.07.026
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SCLC患者#
32
#THORAC#
26
#CNS#
50
#转移灶#
39
#NSCLC患者#
31
听起来
65
赞
56
谢谢梅斯提供这么好的信息,学到很多
53
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
54
#奥希替尼#厉害
105