ESC 2014:亚洲急性冠脉综合征(ACS)患者中抗栓治疗管理模式的长期随访(EPICOR-Asia研究)
2014-08-31 丁香园 丁香园
EPICOR-Asia观察性研究是迄今为止关于抗栓策略和临床(缺血-出血)、经济学、生活质量的最大注册研究,将关注ACS患者的临床真实治疗情况及其预后,评估不同治疗模式在临床实践中的潜在风险与获益。研究将入选包括中国、韩国、印度在内的亚太区8个国家219个中心共13000余例ACS患者,其中包括8000名中国患者,评估不同治疗模式在实际临床实践中对患者预后的影响,同时也评估了其对于疾病经济负担和对
EPICOR-Asia观察性研究是迄今为止关于抗栓策略和临床(缺血-出血)、经济学、生活质量的最大注册研究,将关注ACS患者的临床真实治疗情况及其预后,评估不同治疗模式在临床实践中的潜在风险与获益。研究将入选包括中国、韩国、印度在内的亚太区8个国家219个中心共13000余例ACS患者,其中包括8000名中国患者,评估不同治疗模式在实际临床实践中对患者预后的影响,同时也评估了其对于疾病经济负担和对生活质量的影响。EPICOR-Asia及相关的纳入10000例患者的欧洲研究为ACS抗栓治疗提供了一个大规模的数据库,关于临床结果的随访更是长达2年。目前已取得了一定的研究成果,并能为亚洲及中国提供当前最亟需的数据。
一.ACS死亡率死亡率居高不下的原因:
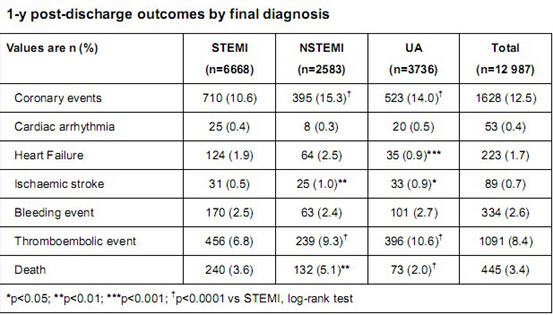
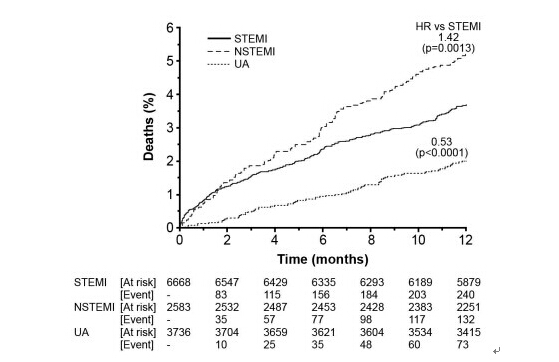
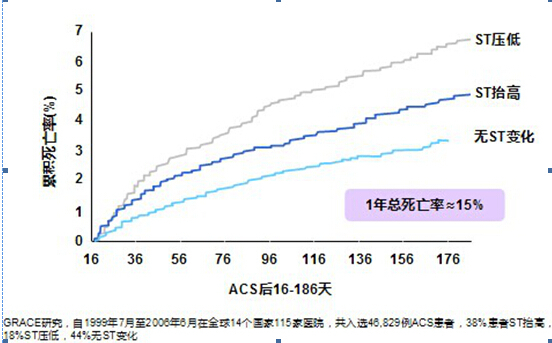
EPICORE-Asia经过长期的数据采集分析发现,目前ACS患者死亡率仍不容乐观。GRACE研究是一项英国和比利时医疗中心前瞻性招募ACS患者并中位随访5年的研究,其数据表明:尽管ACS治疗策略不断规范化,但6个月死亡率仍较高;无论临床表现如何,ACS1年死亡率均较高,约15%,而ACS患者5年累积死亡率高达20%。China Peace研究说明院内STEMI患者死亡率是7%,而EPICOR Asia 表明出院后到1年总的冠脉事件发生率为12.5%,其中死亡率仍然有3.4%,同时血栓性事件发生率为8.4%。
通过设计分析,EPICORE-Asia将影响ACS转归/死亡的不规范管理/危险事件的原因:我国对于ACS的公众教育不足,造成诊断不够及时;患者院前药物使用率较低,院前处理不够完善;并发症未能及时处理;危险因素未充分控制;以及氯吡格雷存在人群的变异性,低反应或抵抗,药物相互作用(PPI)、前体药物起效慢等。
二.替格瑞洛与ACS死亡率之间的关系
纵观全球及中国流行病学数据,ACS死亡率仍不容乐观。
亚洲ACS治疗院前流程还较为落后,病人就医不及时,诊断和药物治疗也不够及时;尽管当前氯吡格雷的使用较为广泛,但ACS患者住院死亡率和长期死亡率仍无显著改善。
多项研究证实,氯吡格雷、普拉格雷尽管降低了心血管事件的复合终点,但遗憾未能进一步降低(心血管)死亡率:
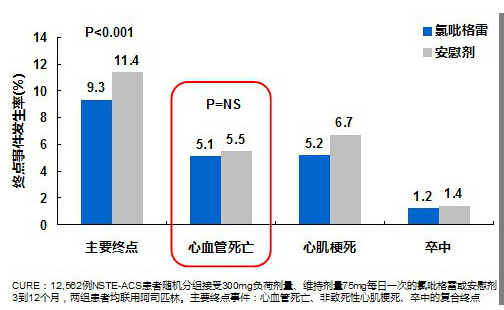
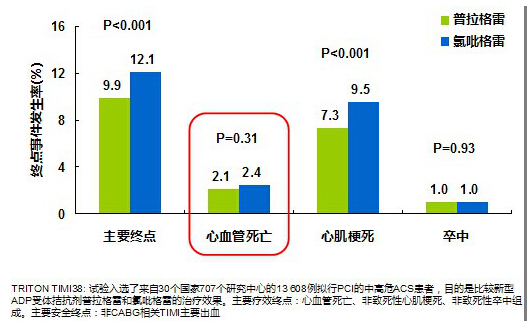
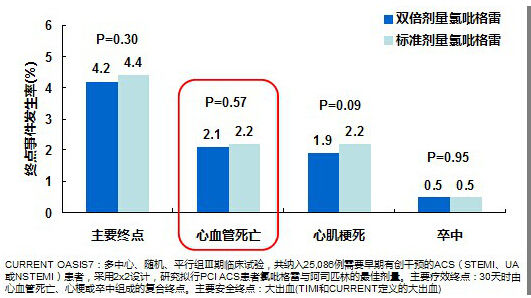
由上图可知,氯吡格雷未能进一步降低(心血管)死亡率,也未能进一步降低PCI患者心血管死亡率,即使氯吡格雷剂量加倍,亦未能降低(心血管)死亡率,亦未
能降低PCI患者(心血管)死亡率。普拉格雷也未能进一步降低(心血管)死亡率。普拉格雷对比氯吡格雷无显著降低心血管死亡率。
ESC指南指出,替格瑞洛是唯一被证实在阿司匹林基础上,进一步降低ACS患者1年心血管死亡率的口服抗血小板药物:
根据EuroPCR 2014上报告的丹麦真实世界研究,替格瑞洛较氯吡格雷显著降低1年心源性死亡率,故替格瑞洛被证实在阿司匹林基础上进一步降低ACS患者1年心血管死亡率的口服抗血小板的唯一药物。
替格瑞洛独特的作用机制(即抑制腺苷摄取)可能带来了其显著的生存获益:
替格瑞洛双重抑制P2Y12受体和腺苷摄取:一方面通过抑制抑制P2Y12受体,起到了很好的抗血小板作用;另一方面,通过抑制红细胞上ENT-1对腺苷再摄取,加强局部腺苷反应,达到额外的血小板聚集/活化抑制作用,以及血管舒张、心肌保护等作用。同时,腺苷在局部组织浓集可能在部分敏感病人中引起一过性的呼吸困难。
替格瑞洛的双途径作用机制带来了其潜在的临床获益,替格瑞洛是唯一在阿司匹林基础上,进一步降低ASC患者心血管死亡率的口服抗血小板药物。希望通过EPICORE-Asia研究,能深刻地了解ACS患者治疗的现状,从中找到更适合中国ACS患者综合治疗的合理模式,也让更多的ACS患者从中受益。
EPICORE-Asia的简介:
在我国,每年有近百万新增的急性冠脉综合症(ACS)患者,其发病率与死亡率均居于高位,而国内目前对ACS患者的数据多来源于临床研究,对ACS院前管理、诊疗路径、药物使用、长期随访的死亡率等的数据研究具有一定的局限性。而为了解决历时长、研究数据不够真实等困难,2011年6月,由中华医学会心血管分会主任委员霍勇教授牵头启动了“在亚洲急性冠脉综合征患者中抗血栓治疗管理模式的长期随访”(EPICORE-Asia)研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PICO#
39
#长期随访#
36
#ASIA#
30
#ACS#
28
#综合征#
23
#管理模式#
26