Hepatology:乙肝肝移植术后恩替卡韦单药治疗长期预后
2017-04-03 MedSci MedSci原创
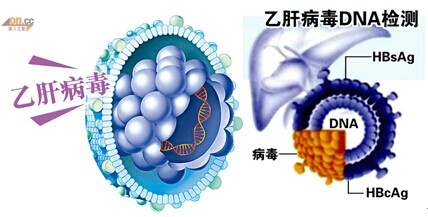
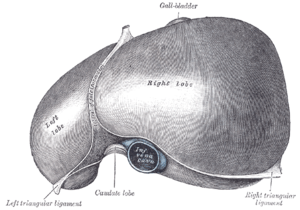
背景:慢性乙型肝炎(CHB)的患者肝移植后,长期抗病毒治疗对预防乙肝复发是必须的。方法:我们观察265例未使用乙肝免疫球蛋白(HBIG)恩替卡韦单一药物治疗的乙型肝炎(CHB)肝移植患者的长期预后。期间定期进行病毒血清学、病毒载量和肝脏生化指标检测。结果:中位随访时间为59个月。累积乙型肝炎表面抗原(HBsAg)血清学清除率在1年和5年时分别为90%和95%。1、3、5、8年HBsAg阴性率分别为
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#单药治疗#
31
#长期预后#
35
#移植术#
32
#恩替卡韦#
37
#EPA#
33