震撼:CAR-T细胞疗法CTL019在2期r/r ALL临床试验中获得93%的完全应答率
2015-12-10 吕顺 美中药源
日前在第57届美国血液学年会(ASH)上报道,制药巨头诺华CAR-T细胞疗法CTL019在一个有59例复发或难治性急性淋巴细胞白血病(r/r ALL)儿童或年轻成年患者参与的2期临床试验中取得了难以置信的93%完全应答率(55/59)。1年生存率为79%(95% CI, 69-91%),其中55%的患者保持完全缓解12个月以上(95% CI, 42-73%)。这些患者之前都接受过标准疗法治疗没有应
日前在第57届美国血液学年会(ASH)上报道,制药巨头诺华CAR-T细胞疗法CTL019在一个有59例复发或难治性急性淋巴细胞白血病(r/r ALL)儿童或年轻成年患者参与的2期临床试验中取得了难以置信的93%完全应答率(55/59)。1年生存率为79%(95% CI, 69-91%),其中55%的患者保持完全缓解12个月以上(95% CI, 42-73%)。这些患者之前都接受过标准疗法治疗没有应答或多次复发。该临床试验在费城儿童医院(CHOP)进行,这是至今为止治疗复发或难治性ALL儿童或年轻成人患者的最大CAR-T临床试验。ASCO也有报道(ASCO 2015:CAR-T治疗药物CTL019难治性非霍奇金淋巴瘤疗效潜力惊人)。如果不出意外,诺华将在2016年向FDA递交CTL019的上市申请,并有望在2017年甚至更早获得FDA批准。
急性淋巴细胞白血病(ALL)起源于淋巴细胞,是一种B或T细胞在骨髓内异常增生引起的恶性肿瘤。这些异常增生的细胞不仅在骨髓聚集并抑制正常造血功能,同时也可侵及骨髓外的组织,如脑膜、淋巴结、性腺、肝等。0~9岁的儿童是ALL的高发人群,占儿童白血病的70%以上。随着造血干细胞移植和联合化疗的逐步完善,早期ALL患者的治疗获得较好疗效,大约80%的儿童和30%的成人能够获得长期无病生存,并且有治愈的可能。但遗憾的是也有一些难治性患者对现有疗法不应答或治疗之后迅速复发,而这些复发或难治性患者的预后非常差,平均生存期通常不到一年。
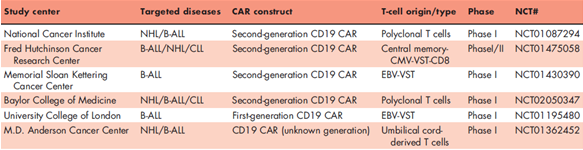
嵌合抗原受体T细胞免疫疗法(Chimeric Antigen Receptor T-Cell Immunotherapy,CAR-T)是制药工业近期最重要的颠覆性发现之一。CAR-T疗法通过采集患者的外周血并提取T细胞,把病人的免疫T细胞在体外通过生物技术改造,令其识别肿瘤细胞表面的抗原,然后把这些细胞输回给病人,达到识别、杀死癌细胞的治疗效果。比如CTL019是把患者的T细胞加上识别B细胞表面抗原CD19以及CD3和CD137(4-1BB)这两个激活T细胞的信号接收蛋白域偶联而成。因为CD19主要在B细胞表达所以CTL019副作用相对较小。CAR-T细胞疗法和传统疗法的另一个主要区别是它进入人体后还会继续繁殖。比如宾夕法尼亚大学的Carl June在2010年为一个6岁的白血病小女孩,艾米丽•怀特黑德进行了CAR-T细胞疗法,现在经过了5年她体内依然还有这种改造过的白细胞存在。也就是说即使癌症复发,这些依然存在的有效T细胞也能把重新出现的癌细胞杀死,在一定程度上解决了癌症复发的问题。
CTL019日前报道的2期临床结果和之前只有一半病例参与的1期临床结果(完全缓解率92%,36/39)几乎完全相同。不良事件的发生率也非常相似,88%的患者(52/59)出现1-4级的细胞因子释放综合征(CRS),表现为高烧、恶心、肌肉疼痛等炎症反应,有时还会出现低血压和呼吸困难。其中大约四分之一需要治疗,但所有症状经过IL-6受体拮抗剂tocilizumab治疗后都得到逆转。CTL019在2014年7月获得美国FDA的突破性药物认定,治疗复发或难治性的ALL。
除了细胞因子风暴以外,CAR-T细胞疗法的广泛推广还受到其它挑战。比如CAR-T疗法不是传统的药物,其治疗程序非常复杂,不仅需要培训高级的专业人员,对临床设施的要求也非常高。在美国一次CAR-T的治疗成本据说高达50万美元以上。如何把目前专业人员处理的、复杂的、高门槛的整个过程自动化、流程化,减少成本是CAR-T疗法获得广泛应用的一个主要挑战。CAR-T另一个亟需解决的问题是到目前为止CAR-T的巨大成功还仅限于血液肿瘤,而在更多的90%固体肿瘤中疗效欠佳。比如在一个靶向HER2的CAR-T细胞疗法CART-meso的一个1期临床试验中,最先使用CART-meso的6个病人没有应答,但有4例在用药4周后病情稳定。所以实体瘤疗效是CAR-T疗法的又一个关键门槛。如论如何,CAR-T细胞疗法都是制药工业当之无愧的颠覆性发明。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
35
好文章,值得看。
113
赞
57
#Car-T细胞疗法#
34
#ALL#
29
#T细胞疗法#
31