Gastroenterology:肝硬化Child-PughA或B级患者应用辛伐他汀或具生存获益(附MedSci解读)
2016-06-04 MedSci MedSci原创
西班牙一项研究表明,查尔德-皮尤(Child-Pugh)A或B级肝硬化患者,标准治疗加用辛伐他汀未能减少食管胃底静脉曲张再出血风险,但与患者的生存获益相关。论文发表于《胃肠病学》杂志5月刊[Gastroenterology 2016,150(5):1160]。该多中心、双盲、随机对照试验共纳入158例接受标准预防静脉曲张再出血治疗(β-受体阻滞剂和套扎)的肝硬化患者。在出血10天内,受试者依据Ch
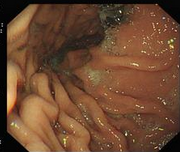
西班牙一项研究表明,查尔德-皮尤(Child-Pugh)A或B级肝硬化患者,标准治疗加用辛伐他汀未能减少食管胃底静脉曲张再出血风险,但与患者的生存获益相关。论文发表于《胃肠病学》杂志5月刊[Gastroenterology 2016,150(5):1160]。该多中心、双盲、随机对照试验共纳入158例接受标准预防静脉曲张再出血治疗(β-受体阻滞剂和套扎)的肝硬化患者。在出血10天内,受试者依据Child-Pugh A或B对C级分层,随机予辛伐他汀或安慰剂治疗。随访24个月。主要终点为再出血和死亡。结果显示,安慰剂和辛伐他汀组分别有30例和22例患者出现主要终点事件(P=0.423);两组的死亡率分别为22%和9%[风险比(HR)为0.39,95%CI:0.15-0.99, p=0.030]。辛伐他汀未能改善Child-Pugh C级患者的生存率;两组的再出血发生率分别为28%和25%(p=0.583);严重不良事件发生率分别为53%和49%(P = 0.752),治疗相关性严重不良事件发生率分别为11%和8%(P = 0.599)。辛伐他汀组有2例晚期肝病患者发生横
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Child-Pugh#
29
#ILD#
26
#AST#
23
#Gastroenterol#
27
#生存获益#
27
#GAS#
28
#child#
31
怎么能想到研究他汀类药物对出血的影响呢?
101
#辛伐他汀#
29
#Gastroenterology#
18