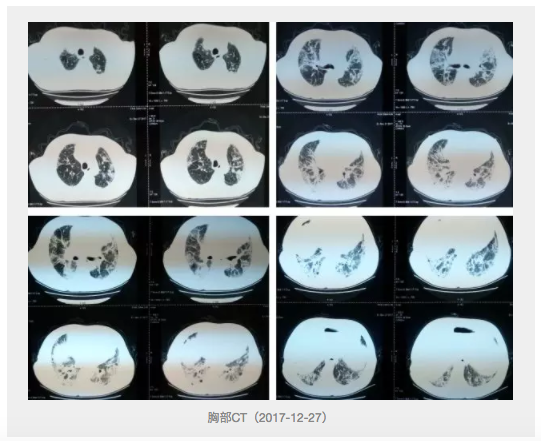
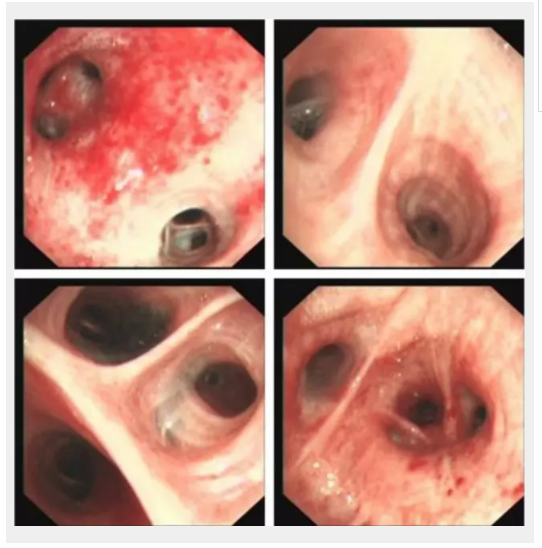
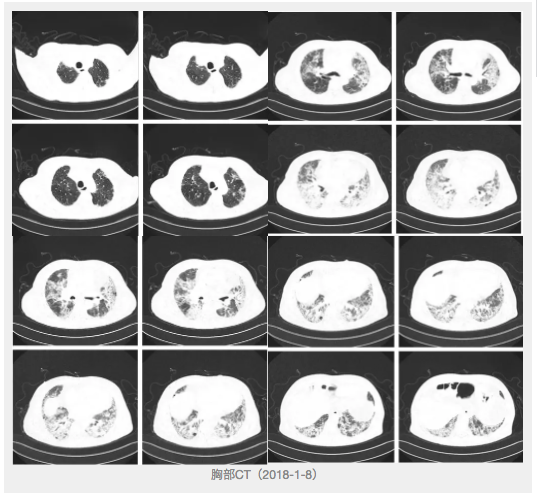
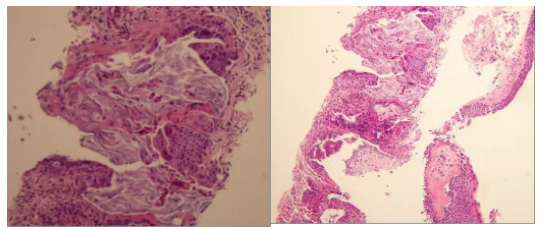
病例分享:患者因气短被诊断为间质性肺病,没想到背后还有肺癌等着?重重迷雾下哪些因素或是漏诊误诊的帮凶?
2018-03-29 兰州大学第一医院老年呼吸科 谭恩丽、包海荣 呼吸界
间质性肺病(Interstitial lung disease,ILD)是一大类肺部疾病的统称,不仅累及肺间质,也可累及肺实质。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习啦🙏
18
#间质性#
35
#漏诊误诊#
23
#肺病#
35
学习了.谢谢作者分享!
60
学习了.谢谢作者分享!
51
学习了.谢谢作者分享!
58
学习了
59
好文献.学习了
62
#漏诊#
31