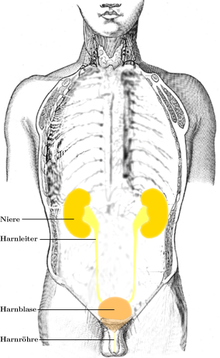
Sci Rep:CDKN2A可以作为肌肉侵入性膀胱癌风险分层和治疗决定的转录组标记
2018-10-12 AlexYang MedSci原创
细胞周期控制基因CDKN2A的缺失被描述为侵入性膀胱癌的恶化标记,并且与成纤维细胞生长因子(FGFR3 )的变异有关。CDKN2A RNA表达在肌肉侵入性膀胱癌(MIBC )中的预后作用仍旧需要研究。最近,有研究人员在80名MIBC且经历根治性前列腺切除的患者中对CDKN2A和FGFR3的表达进行了qRT-PCR分析(测试组)。MDA组(n=8)和TCGA组(n=365)用于进行验证。研究发现,药
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#转录#
33
#癌风险#
23
#侵入性#
32
#风险分层#
0
#转录组#
29
#CDK#
28