Eur Heart J:微血管性心绞痛患者的临床特征和预后
2021-05-27 MedSci原创 MedSci原创
这项国际研究提供了新的证据,即无论性别或种族,MVA都是重要的健康问题,并且女性MVA患者的生活质量较男性低,尽管两者预后相当。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在明确微血管性心绞痛(MVA)患者的临床特征和预后。
冠状动脉血管舒缩性疾病国际研究小组提出了MVA的诊断标准。研究人员根据这些标准及其预后对患者的临床特征进行了前瞻性评估。该研究的主要终点是主要心血管事件(MACE)的复合事件,其中包括心血管死亡、非致命性心肌梗塞、非致命性卒中以及因心力衰竭或不稳定型心绞痛导致的住院。

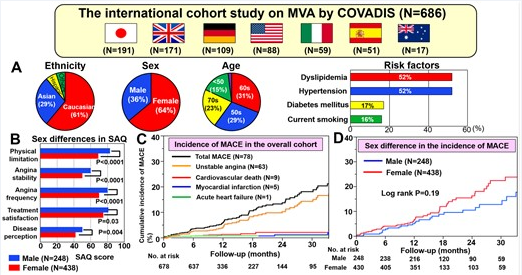
在2015年7月1日至2018年12月31日期间,来自4大洲7个国家/地区的14个机构登记了686例MVA患者。其中,女性占64%,主要族裔是白种人(61%)和亚洲人(29%)。
微血管性心绞痛患者的临床特征和预后
在平均398天的随访期间(IQR为365-744),共有78例MACE(男性为6.4%,女性为8.6%,P=0.19)。多变量Cox比例风险分析表明,高血压和既往冠状动脉疾病史(CAD),包括急性冠状动脉综合征和稳定型心绞痛在内,是MACE的独立预测因子。尽管女性的西雅图心绞痛问卷得分低于男性,但患者预后没有性别或种族差异(P<0.05)。
由此可见,这项国际研究提供了新的证据,即无论性别或种族,MVA都是重要的健康问题,并且女性MVA患者的生活质量较男性低,尽管两者预后相当。
原始出处:
Hiroaki Shimokawa.et al.Clinical characteristics and prognosis of patients with microvascular angina: an international and prospective cohort study by the Coronary Vasomotor Disorders International Study (COVADIS) Group.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab282
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管性#
48
#临床特征#
38
#ART#
42
#微血管#
34
#HEART#
50
学习了
65
每日一看
62