Neurosurgery:静脉性搏动性耳鸣
2021-12-23 ANDs 网络
耳鸣是一种在没有外界刺激的情况下对声音的异常感知。静脉性搏动性耳鸣(Venous pulsatile tinnitus,VPT)是一种特殊形式的耳鸣,其特征是由于局部静脉异常而产生的客观和主观杂音。
耳鸣是一种在没有外界刺激的情况下对声音的异常感知。静脉性搏动性耳鸣(Venous pulsatile tinnitus,VPT)是一种特殊形式的耳鸣,其特征是由于局部静脉异常而产生的客观和主观杂音。临床评估依赖于声音质量、持续时间和诱发因素。特发性颅内高压(Idiopathic intracranial hypertension,IIH)和横窦狭窄(transverse sinus stenosis,TSS)是VPT最常见的原因。其他原因包括乙状窦壁异常(sigmoid sinus wall abnormalities,SSWA)、颈静脉异常(jugular vein anomalies,JVAs)和导静脉异常。这些异常可以在磁共振成像、磁共振血管造影/磁共振静脉造影和高分辨率颞骨计算机断层扫描中检测到。VPT背后的发病机制包括管腔狭窄或异常扩张导致的湍流、颞骨缺损导致的内部声音放大以及临近听觉骨结构静脉窦结构的位置异常。基于这些理论,可以应用不同的介入治疗方式来治疗。对于 IIH 和 TSS 患者,可以采用血管内横窦支架置入、SSWA和JVA弹簧圈栓塞以及异常导静脉的栓塞等,目前来看是安全和有效的。需要进一步弄清楚这些异常的自然史,以及介入治疗 VPT(不同于其他类型的耳鸣)的疗效。
图1. 54岁,女性,搏动性耳鸣。A、MRV显示双侧横窦狭窄。B、 检眼镜检查显示乳头水肿:
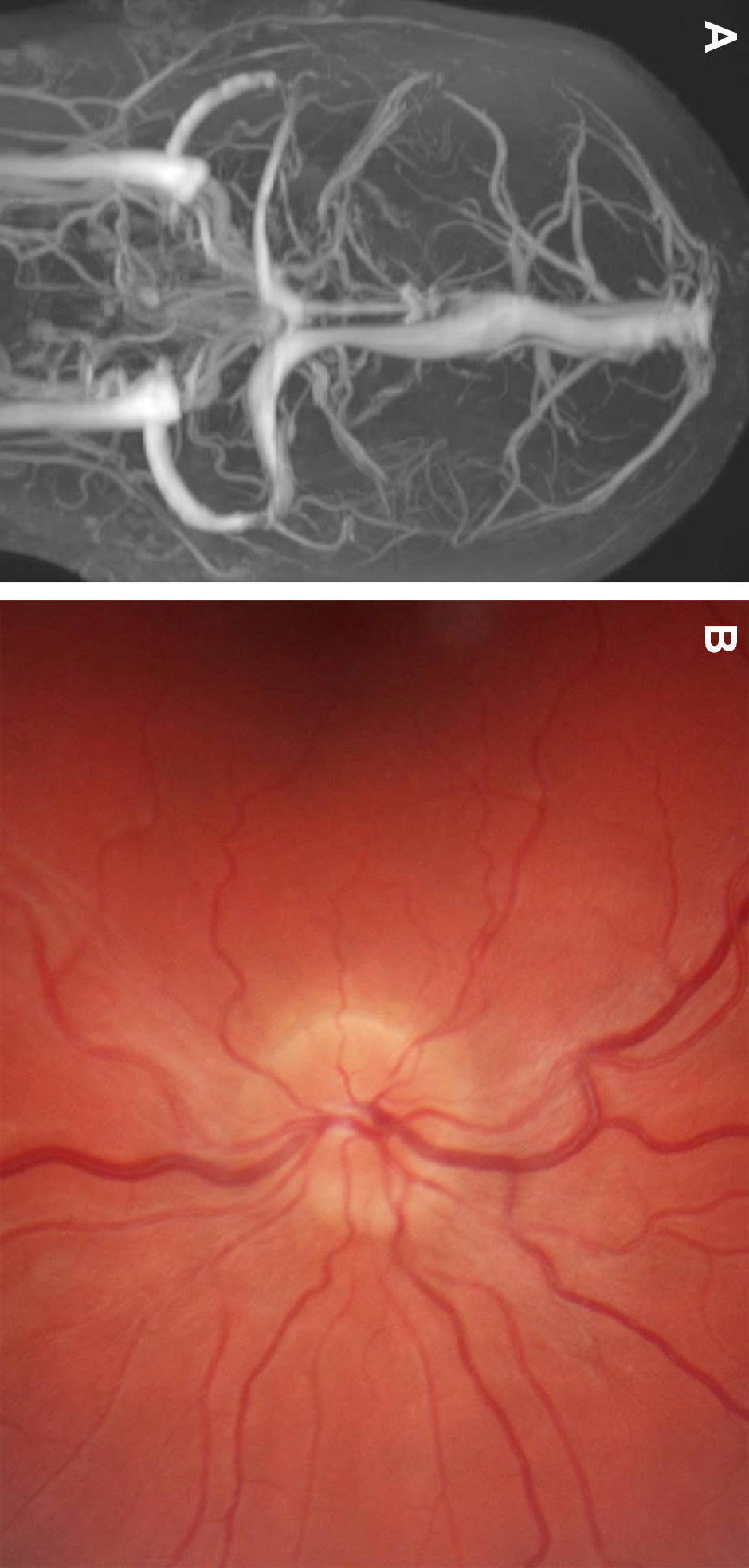
图2. 58岁,6个月的右耳搏动性耳鸣病史,轻度压迫颈部症状缓解。A、CTV显示右乙状窦远端局灶性狭窄。B、轴位CTV显示局灶性充盈缺损,可能是蛛网膜颗粒或慢性血栓。C、脑静脉造影显示右乙状窦远端严重狭窄。狭窄处的压力梯度为14 mmHg。D、放置支架后,重复静脉造影显示狭窄减轻。压力梯度消失。患者在3个月随访时症状消失:

图3. 窦气征(Air on sinus sign)。轴位平扫CT显示乙状窦板裂开(dehiscent sigmoid plate),空气与右乙状窦相邻:

图4. A、CTV显示乙状窦憩室(diverticulum)侵入右颞骨和乳突气房。B、冠状MRV显示憩室。C、常规静脉造影显示憩室内放置一个微导管。D、弹簧圈栓塞后静脉造影显示憩室闭塞:
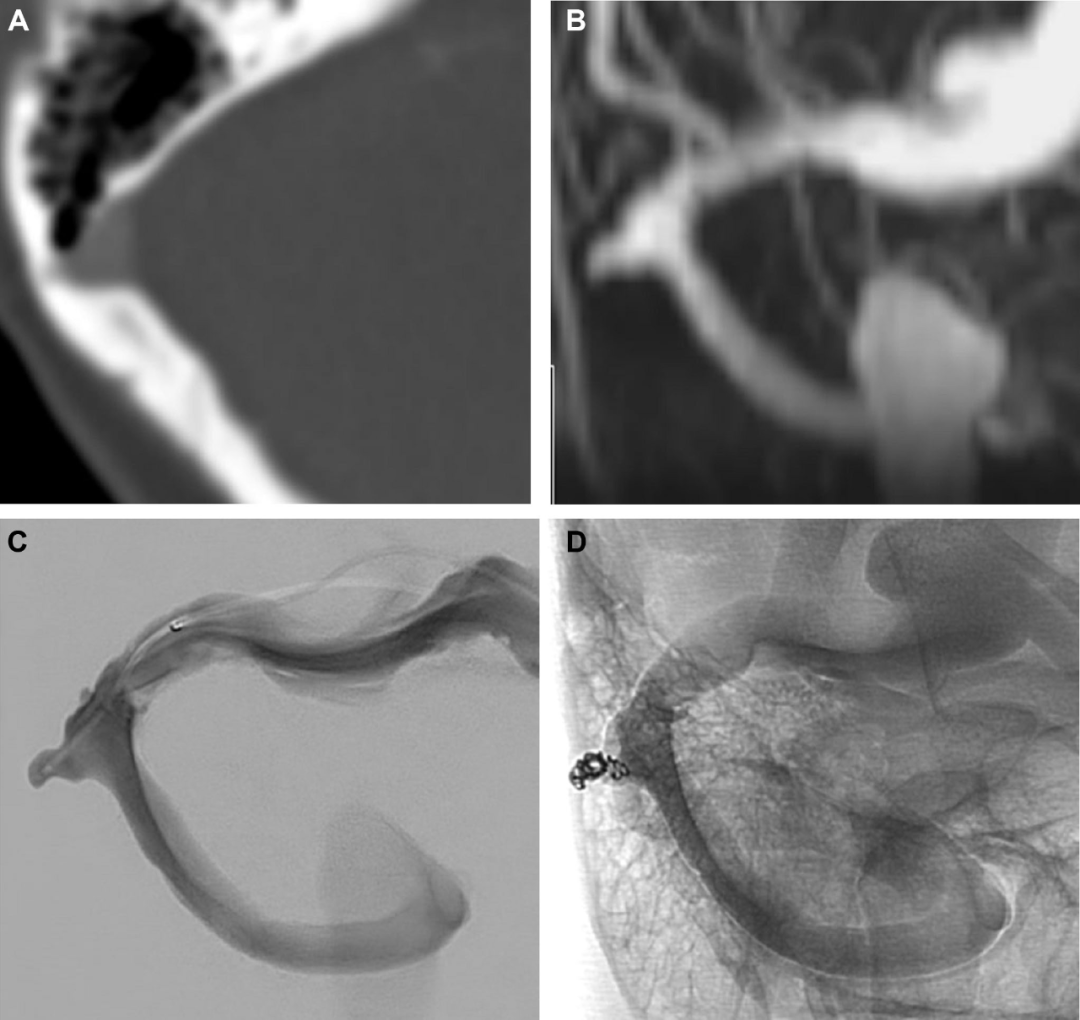
图5. 轴位CT显示右侧乙状窦板(A)比对侧(B)薄:
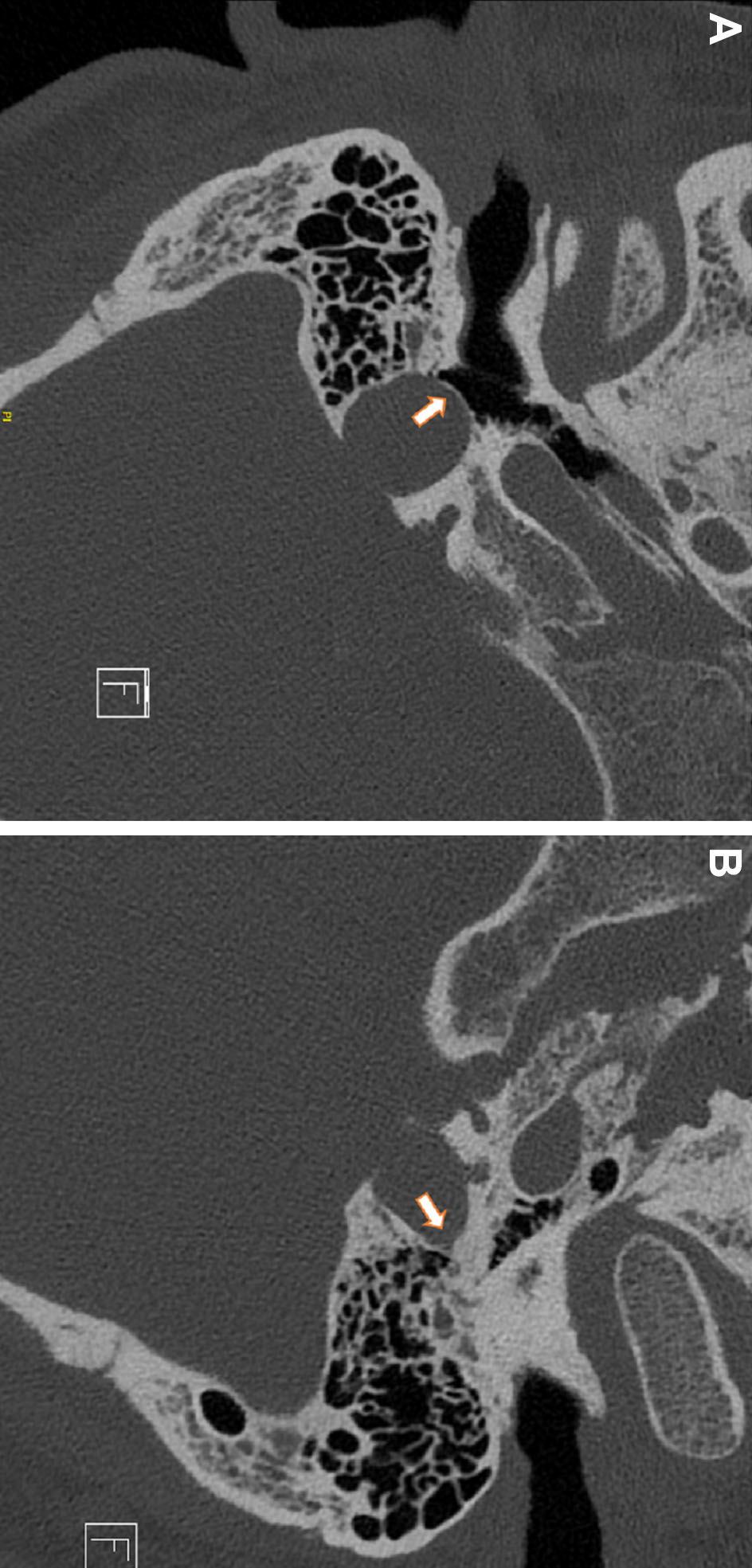
图6. 颈静脉球憩室,鼓膜后血管团。A、耳镜检查显示一个蓝色鼓膜后肿块。B、MRV MIP图像显示右侧颈静脉球憩室(红色箭头)。C、MRV MIP图像显示右侧高位颈静脉球:

图7. MIP MRV图像显示左侧乳突导静脉(绿色箭头)轻度扩张,起自于左侧乙状窦,这种情况通常为无临床意义的正常变异,偶尔可出现搏动性耳鸣:

Neurosurgery. 2021 Oct 13;89(5):760-768.
doi: 10.1093/neuros/nyab299.
Venous Causes of Pulsatile Tinnitus: Clinical Presentation, Clinical and Radiographic Evaluation, Pathogenesis, and Endovascular Treatments: A Literature Review
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
39
#GER#
36
#surgery#
46
#耳鸣#
43
#ROS#
32