Heart:STEMI患者长期死亡率和院前替罗非班治疗!
2017-07-06 xing.T MedSci原创
由此可见,在STEMI患者中,基线血浆NT-proBNP水平可独立预测长期死亡率。基线NT-proBNP水平高于中位数的患者,采用替罗非班早期院前治疗可以显著降低30天和1年死亡率,提示高危患者可能获得特别的好处,这一发现应该在其他研究中予以证实。
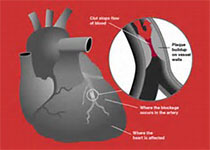
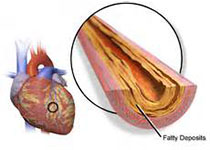
近日,在心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员对安慰剂对照、双盲、随机对照试验的On-TIME 2(正在进行的替罗非班在心肌梗死的疗效评估2)研究进行了亚组分析,以评价氨基末端脑钠肽前体(NT-proBNP)水平与5年死亡率之间的相关性,并探讨院前应用替罗非班对NT proBNP水平相关死亡率的影响。 该研究共纳入了984名接受急诊经皮冠状动脉介入治疗(PCI)的ST段抬高型心肌梗死(STEMI)患者,这些患者被随机分为接受替罗非班或安慰剂治疗。在入院造影前(基线)和之后18-96小时测量了受试者的NT-proBNP水平。 该研究共有918例(93.3%)患者基线NT-proBNP值可用,PCI后有865例(87.9%)患者NT-proBNP值可用。研究人员发现基线NT-proBNP值高于平均值(137 pg/ml)的患者有更高的30天(5.1% vs. 0.2%,P<0.001)、1年(7% vs. 0.7%,P<0.001)和5年(20.3% vs. 4.9%,P<0.001)死亡率,相比于低于中位数的患者。研究人员使用Cox回归分析发现NT
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#院前#
23
#STEMI患者#
28
学习了谢谢分享!
43
#ART#
27
#STEM#
29
#HEART#
18
原文题目呢
45
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
58