Cell Metab:白血病、炎症治疗的新策略
2015-01-09 佚名 生物谷
根据华盛顿大学医学院一项新的研究证实:与糖尿病和肥胖相关的酶可能在关节炎和白血病中发挥关键作用,这就有可能开辟治疗这些疾病的新途径。 利用遗传工程小鼠开展的研究工作,研究人员发现参与将碳水化合物转化为脂肪的酶也影响特定白细胞即中性粒细胞的健康。嗜中性粒细胞是最丰富的类型的白血细胞,其是炎症的标志,而炎症是类风湿关节炎的一个关键组成部分。异常高水平的中性粒细胞在白血病患者也常见。 这项研究发表在
根据华盛顿大学医学院一项新的研究证实:与糖尿病和肥胖相关的酶可能在关节炎和白血病中发挥关键作用,这就有可能开辟治疗这些疾病的新途径。
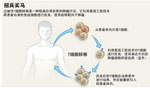
利用遗传工程小鼠开展的研究工作,研究人员发现参与将碳水化合物转化为脂肪的酶也影响特定白细胞即中性粒细胞的健康。嗜中性粒细胞是最丰富的类型的白血细胞,其是炎症的标志,而炎症是类风湿关节炎的一个关键组成部分。异常高水平的中性粒细胞在白血病患者也常见。
这项研究发表在Cell Metabolism杂志上。这些酶和中性粒细胞之间的联系是一个巨大的惊喜,论文第一作者Irfan J. Lodhi博士说:我们从来没有想过通过瞄准产生脂肪酸的酶,来治疗类风湿关节炎或白血病。
在这项研究中,小鼠剔除产生某种类型脂肪所需要酶后,小鼠体重突然降低,并含有极低的白细胞数量,极少数的中性粒细胞。如果没有这个脂肪即醚脂,中性粒细胞会死亡。
该发现提示靶向醚脂,或可降低炎性疾病和白血病嗜中性粒细胞的数量。研究人员认为限制,而不是消除醚脂可能是最好的方法,因为嗜中性粒细胞对于抗感染是重要的。
研究员Clay F. Semenkovich医学博士表示:这可能是限制炎症的一个途径,如果我们能降低这些酶的活性,而不完全消除它们,就可能降低醚脂水平,潜在帮助白血病和炎性疾病患者如关节炎。
Semenkovich说,这些酶特异性地靶向中性粒细胞,而不影响其他的免疫细胞。因此,醚脂似乎是一个非常精确的靶标。研究人员还发现失活这些酶不会损伤中性粒细胞的前体细胞,而只杀死成熟中性粒细胞。这意味着限制醚脂生成的策略有可能只是短暂地降低中性粒细胞水平,因此当治疗终止时,患者的粒细胞数量将逐渐升高,使得免疫系统恢复正常。
原始出处
Lodhi IJ1, Wei X1, Yin L1, Feng C1, Adak S1, Abou-Ezzi G2, Hsu FF1, Link DC2, Semenkovich CF3.Peroxisomal lipid synthesis regulates inflammation by sustaining neutrophil membrane phospholipid composition and viability.Cell Metab. 2015 Jan 6;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
25
#MET#
24
#Cell#
16
#Meta#
21
#炎症治疗#
32
#新策略#
20