Circulation: 应用他汀药物后,血脂和冠心病发生风险之间的相关性减弱
2016-01-23 MedSci译 MedSci原创
背景:2001年胆固醇治疗指南发表后,US冠心病成人中他汀类药物的应用增加。方法:研究者收集REGARDS研究中的9578名受试者及KPSC中346 595人,2003年到2007年间的血脂水平,评估血脂和CHD之间的相关性。研究者也收集了1987到1989 ARIC研究中14 590名受试者的血脂水平,对其进行相同的分析。分析限制在45到64岁间,没有CHD,也没有服用他汀类药物的黑人和白人。基
背景:2001年胆固醇治疗指南发表后,US冠心病成人中他汀类药物的应用增加。
方法:研究者收集REGARDS研究中的9578名受试者及KPSC中346 595人,2003年到2007年间的血脂水平,评估血脂和CHD之间的相关性。研究者也收集了1987到1989 ARIC研究中14 590名受试者的血脂水平,对其进行相同的分析。分析限制在45到64岁间,没有CHD,也没有服用他汀类药物的黑人和白人。基线时,检测受试者总胆固醇,高密度脂蛋白胆固醇和甘油三酯。计算,低密度脂蛋白胆固醇,非高密度脂蛋白胆固醇,总胆固醇和高密度脂蛋白胆固醇,甘油三酯和高密度脂蛋白胆固醇的比例。
结果:在ARIC研究中,低密度脂蛋白较高的患者,糖尿病的患病率、脑卒中病史、和抗高血压药物的使用增加,但在REGARDS和KPSC研究中没有增加。在8.9年的随访中,REGARDS研究中,225例冠心病事件发生,在KPSC研究中, 6547例CHD事件发生,在ARIC研究中,583例冠心病事件发生。多变量校正后,ARIC研究中,不良的血脂水平与冠心病的发生风险较高相关。这些相关性在REGARDS研究和在KPSC研究中减弱。例如,ARIC研究,REGARDS研究和KPSC研究中,最高与最低四分位数的低密度脂蛋白胆固醇(≥146与≤102毫克/分升)的相关的HR分别为:1.89(95%CI,1.42-2.51),1.25(95%CI,0.81-1.92)和1.49(95%CI,1.38-1.61)。
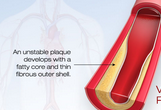
结论:高风险CHD患者中应用他汀类药物,血脂和CHD发生风险之间的相关性可能是下降的。
原文出处:
Colantonio LD, Bittner V, et al. Association of Serum Lipids and Coronary Heart Disease in Contemporary Observational Studies. Circulation. 2016 Jan 19.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#相关性#
26
有道理
92
收藏
112
我仔细看看
126
血脂高的心血管事件
130
血脂,想说爱你不容易
54
这个研究是说明他汀类药物,的降脂的效果,还是说明他汀类药物还有其他的作用?
77
意义何在?
78
牛
84
学习了,希望有更多的循征支持
70