盘点:近期哮喘重要研究一览
2016-08-25 MedSci MedSci原创
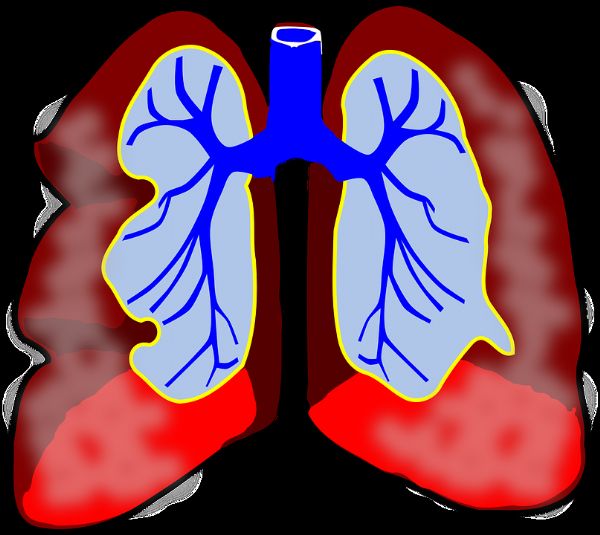
哮喘又名支气管哮喘。支气管哮喘是由多种细胞及细胞组分参与的慢性气道炎症,此种炎症常伴随引起气道反应性增高,导致反复发作的喘息、气促、胸闷和(或)咳嗽等症状,多在夜间和(或)凌晨发生。哮喘是一种具有复杂性状的,具多基因遗传倾向的疾病。其特征为:①外显不全,②遗传异质化,③多基因遗传,④协同作用。近期有关哮喘的大量临床研究,从不同方向、不同角度对哮喘及其并发症的临床诊治进行了深入研究,为哮喘的临床

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













不错哦继续关注
70
这篇资讯总结的真好,有新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。。有帮助的
70
学习起来
74
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
77
学习了,赞一个!!!
67
学习了,赞一个!!!
34
学习了,赞一个!!!
31
学习了,赞一个!!!
19
继续学习
24
继续关注了
26