腰椎间盘突出引起的腰腿痛不算病吗?腰突常见误区
2017-02-25 佚名 搜狐
腰腿痛是很多人尤其是上年纪的人经常出现的症状。有研究指出,约有95%以上的人一生中有过腰腿痛的经历。在我国腰腿疼的患者有2亿左右,其中30-40岁出现腰腿痛的概率为59.1%;50-60岁出现腰腿痛的概率为71%;60岁以上出现腰腿痛的概率达82%。据统计,其中,由于腰椎间盘突出导致的腰腿痛约为15.2%。
腰腿痛是很多人尤其是上年纪的人经常出现的症状。有研究指出,约有95%以上的人一生中有过腰腿痛的经历。在我国腰腿疼的患者有2亿左右,其中30-40岁出现腰腿痛的概率为59.1%;50-60岁出现腰腿痛的概率为71%;60岁以上出现腰腿痛的概率达82%。据统计,其中,由于腰椎间盘突出导致的腰腿痛约为15.2%。

腰腿痛的出现可由多种疾病导致,有些患者症状可在简单治疗之后消失,甚至不治而愈。因此,很多人(尤其是老年人)认为腰腿痛只是人体老话之后正常表现,不是由于疾病导致的症状。真的是这样吗?
重庆医科大学附属第一医院神经外科脊柱脊髓疾病治疗组晏怡教授表示:“腰椎间盘突出引起的腰腿痛不仅算病,而且必须引起高度重视。因为腰椎间盘突出导致的腰腿痛只是早期最常见症状,如果不做治疗放任疾病发展,患者可能出现下肢麻木、无力,甚至瘫痪,大小便障碍,严重影响生活质量。”
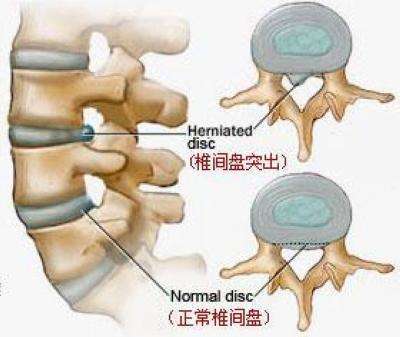
腰椎间盘突出虽然常见,但是很多人对于本病的认识存在误解,比如上述介绍的“腰椎间盘突出引起的腰腿痛不算病”等,那么,还有哪些呢?
有的患者在患病简单查找资料后或腰椎间盘突出不断复发的时候就得出结论:腰椎间盘突出是治不好的!真的是这样吗?
晏怡教授介绍,临床上腰突症治疗的总体效果非常好,优良率约在95%左右。只所以有很多的患者会误以为腰椎间盘突出是治不好的是由于两点原因:一、没有接受正确诊疗;二、没有坚持治疗。
有很多的患者在就诊时都会询问:医生,为什么不给我牵引(按摩、手术……)那xxx就是牵引治好的啊!
晏怡教授表示:“腰椎间盘突出治疗选择较多,但是并不是任意选择一种方式都能够治愈患者,而是有着其严格适应症的,患者在疾病的治疗中需谨记‘甲之蜜糖’可能是‘乙之砒霜’适合别人并不一定适合你,正确的态度是根据临床症状、体征、病程,影象学检查选择适合每一个患者的具体治法。”
临床上,腰椎间盘突出患者关于手术的误解是最多的,通常可以分为两类:一、“手术万能论”;二、“手术无用论”。“手术万能论”是很多的患者在就诊的时候不顾自己病情,不顾是不是存在手术适应症,盲目的要求手术,忽视手术风险等;“手术无用论”是与之相对的一类患者,此类患者认为“小小”腰椎间盘突出没有必要手术,殊不知如果腰突造成脊髓或神经受到压迫的话,手术是唯一有效的治疗方式。
晏怡教授表示:“只有正确认识疾病,才能更好的治疗疾病,因此腰椎间盘突出患者患病只有一定要避免误区,及时到神经外科接受诊疗,避免误诊、误治。”
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#椎间盘突出#
36
#腰腿痛#
37
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。
49
文意真好,值得分享
56
讲了等于没讲
44
#腰椎#
22
#误区#
31
#腰椎间盘#
25