【一般资料】
患者,男,8岁
【主诉】
因身材发育矮小瘦弱、手足短小来就诊。
【体格检查】
发育矮小,营养良好,智力发育正常,双肺呼吸音清晰,心脏各瓣膜区未闻及杂音。腹软,肝脾未及。四肢发育短小,尤以手足明显。患者实验室各项检查未见异常。
【辅助检查】
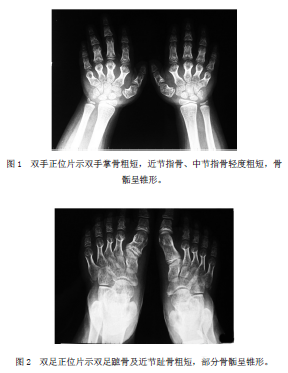
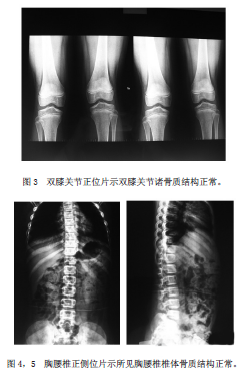
双手、双足、双膝正位及胸腰椎正侧位摄片。X线片显示患儿双手掌骨、双足蹠骨粗短,近节指骨、中节指骨轻度变粗短,手足短骨干骺端呈杯口状,骨骺成锥形,上述骨虽粗短,但无畸形,骨质结构亦正常,双侧腕骨、跗骨正常(图1、2)。双膝关节、胸椎、腰椎X线片示双膝诸骨及胸、腰椎骨质正常(图3、4、5)。X线诊断为周围型骨发育障碍。周围型骨发育障碍为一种少见的常染色体显性遗传疾病,病因不明,最早由Brailsford进行报道。周围型骨发育障碍临床特点:患者身材矮小,躯干与四肢比例正常,手足诸骨发育粗短,患者一般婴儿期生长发育基本正常,常于出生一年后患儿家长发现患儿手足短小就诊。周围型骨发育障碍病理改变主要是手足软骨发育不全,干骺端缺少正常排列的软骨细胞柱,软骨生长障碍,骨化不良,导致手足管状骨纵向生长缓慢,尤以边缘为著;同时膜内化骨正常,骨骺骨化中心向凹陷的干骺端延伸,形成锥形。患者手足粗短可能因手足干骺端软骨发育障碍及骨骺提前愈合所致。患者肢体无其它异常,智力正常,血生化检查正常。有报道称周围型骨发育障碍可合并听觉障碍、蓝眼睛。该病典型X线表现为双侧对称性掌骨、蹠骨粗短明显,而近节指骨、中节指骨相对较轻,虽然变短,但无畸形,骨质结构正常。双侧手足短管状骨干骺端可呈杯口状改变,骨骺呈锥形。双侧腕骨、跗骨大小形态正常,但成熟加速。鉴别诊断周围型骨发育障碍需与小儿软骨发育不全及粘多糖病(Ⅰ型、Ⅳ型)鉴别诊断。(1)小儿软骨发育不全为全身所有软骨内化骨的部位均出现对称性异常,长管骨粗短且弯曲,骨皮质增厚尤以弯曲的凹侧更为明显,干骺端增宽,向两侧张开,中央凹陷呈“杯口状”或“V”型,骨骺被其包围,此表现以膝部显著;椎体前部较小,后缘轻度凹陷,前缘轻度向前凸呈弹头样改变,腰椎椎弓根间距1-5逐渐变小(正常增大)。(2)粘多糖病Ⅰ、Ⅳ型,腕骨骨化中心出现迟缓,掌骨近端及指骨远端变尖,尺桡骨远端关节面相对倾斜;胸腰段后突畸形,粘多糖Ⅰ型第一腰椎或第二腰椎发育不良、变小及向后移位,脊柱以该处为中心向后突成角畸形,该椎体前缘上部缺如,下部呈喙状突出。粘多糖Ⅳ型椎体普遍性扁平,椎体横径及前后径均增加,椎间隙相对增宽,上述改变胸椎比腰椎明显,椎体表面不规整,椎体前部上下角缺损,使椎体呈楔形变或中部呈舌状前凸。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发育障碍#
48
#发育#
22
学习了新知识
50
学习
57
好病例.谢谢分享.
51