Stroke:TMAO水平与缺血性卒中复发相关(CNSR-III研究)
2021-12-12 brainnew神内神外 网络
王拥军教授团队利用第三次中国国家卒中登记研究(Third China National Stroke Registry, CNSR-III)队列,探讨了不同病因亚型下血浆氧化三甲胺与缺血性卒中复发之间
氧化三甲胺(Trimethylamine N-oxide,TMAO)是一种肠源性的菌群相关代谢产物,近年来被发现是心血管疾病和其他慢性疾病的潜在风险因子,其主要通过增加巨噬细胞中胆固醇的积累和泡沫细胞的形成、促进动脉壁的炎性反应和增加血小板高反应性等发挥致动脉粥样硬化作用。不仅如此,研究还发现TMAO与糖尿病、高血压甚至心房颤动等疾病高度相关。而缺血性卒中作为一种异质性疾病,发病机制多样。基于此,王拥军教授团队利用第三次中国国家卒中登记研究(Third China National Stroke Registry, CNSR-III)队列,探讨了不同病因亚型下血浆氧化三甲胺与缺血性卒中复发之间的关系。
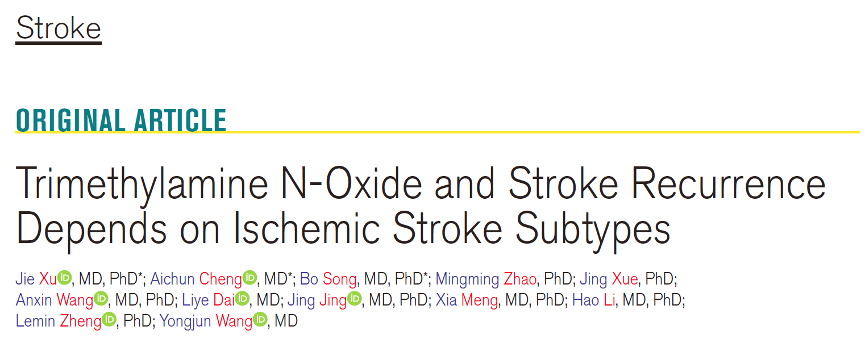
研究共纳入CNSR-III中具有基线TMAO值的10756例缺血性卒中/TIA患者,将患者按照血浆TMAO水平高低分为4组(Q1:<1.17umol/L;Q2:1.17-1.75umo/L;Q3:1.75-2.63umol/L;Q4:>2.63umol/L)。主要研究结局为随访1年内的卒中复发。研究结果发现血浆TMAO水平是1年内卒中复发风险的独立预测因素(Q4 vs Q1:校正HR,1.37;95%CI,1.15-1.64)。进一步根据TOAST分型分层,结果发现血浆TMAO水平与小动脉闭塞型(SAO)患者(校正HR,1.43;95%CI,1.03-2.00) 卒中复发存在相关性,而在大动脉粥样硬化型(LAA)(校正HR,1.19;95%CI,0.95-1.48)、心源性栓塞型(CE)(校正HR,1.54;95%CI,0.95-2.48)和其他型(others)(校正HR,1.19;95%CI,0.98-1.44)中未见明显的相关性。
缺血性卒中作为高复发性、高致残性疾病,积极发现更多潜在影响卒中复发的危险因素,对于缺血性卒中基于不同病因分型的精准治疗及二级预防至关重要。该研究表明血浆TMAO是1年内卒中复发风险的独立预测因素,而对不同TOAST分型的卒中患者其影响存在差异,TMAO增加小动脉闭塞型卒中患者复发风险未来仍需进一步的研究证实。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#缺血性卒#
42
#缺血性#
30
#CNS#
52
#III#
41
#卒中复发#
45
#TMAO#
26