Cell:读取路径≠储存路径?或为治疗阿尔茨海默病提供新思维
2017-08-21 佚名 生物探索
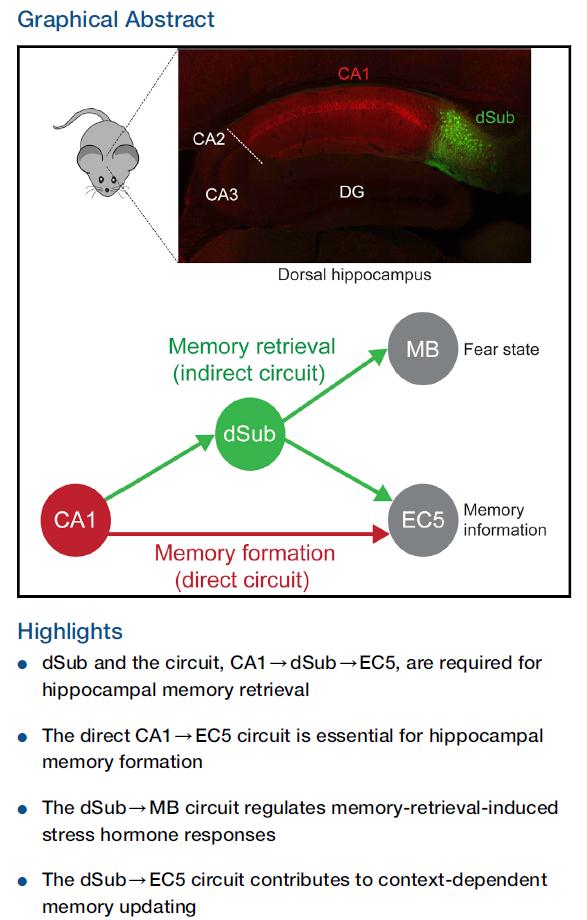
神经科学家一直认为,记忆形成与记忆召回时使用的是同一条神经环路,但近日,一项发表于Cell上的研究颠覆了这一观点。MIT的神经科学家首次表明,记忆召回需要一个“绕道”环路,它不同于原始的记忆形成环路,而是从其中分支出来。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
38
#Cell#
31
#阿尔茨#
31
#阿尔茨海#
30
#阿尔茨海默#
28
路径的研究.目前也越来越多-
73