Nat Commun:新型WNT抑制剂有望清除癌症干细胞用于结直肠癌治疗
2016-08-29 佚名 生物谷
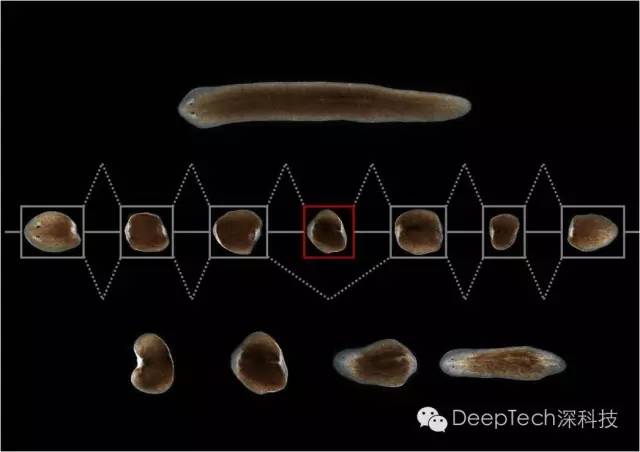
近日,包括日本国家癌症中心在内的多家科研机构联合发表文章,宣布开发出一种叫做NCB-0846的小分子Wnt抑制剂。Wnt信号途径是癌症干细胞发育的一条关键途径,这种抑制剂的出现或为药物难治性结直肠癌病人提供新的治疗选择。 结直肠癌是导致癌症死亡的一个重要原因,全世界每年有大约70万人死于该病。超过90%的结直肠癌携带Wnt信号途径的体细胞突变,比如APC肿瘤抑制基因,导致Wnt信号途径的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
30
#Nat#
22
#癌症干细胞#
28
#结直肠#
31
#WNT#
24
#抑制剂#
26