Clin Cancer Res:Lacnotuzumab联合吉西他滨-卡铂治疗晚期三阴性乳腺癌
2021-12-09 Nebula MedSci原创
Lacnotuzumab+吉西他滨+卡铂治疗晚期三阴性乳腺癌的效果与单用吉西他滨+卡铂的相当。
三阴性乳腺癌 (TNBC) 约占所有乳腺癌的15%-20%。根据指南,TNBC的定义是通过免疫组化检测雌激素受体 (ER) 和孕酮受体 (PgR) 的表达都≤1%。与其他类型的乳腺癌相比,TNBC通常具有更高的转移潜力和更具侵袭性的临床过程。
Lacnotuzumab (MCS110)是一种中和性人源IgG1 κ单克隆抗体,可与CSF1结合,阻断CSF1-介导的受体激活。
本研究是一项II期临床试验,旨在评估在吉西他滨和卡铂的联合方案中加用Lacnotuzumab用于晚期TNBC患者的疗效。
招募了不适合手术或放疗进行治愈性治疗的肿瘤相关巨噬细胞水平较高的晚期TNBC女性患者,予以吉西他滨+卡铂联合或不联合Lacnotuzumab治疗,直到出现不可耐受的毒性、病情进展、医生或患者决定停止治疗。
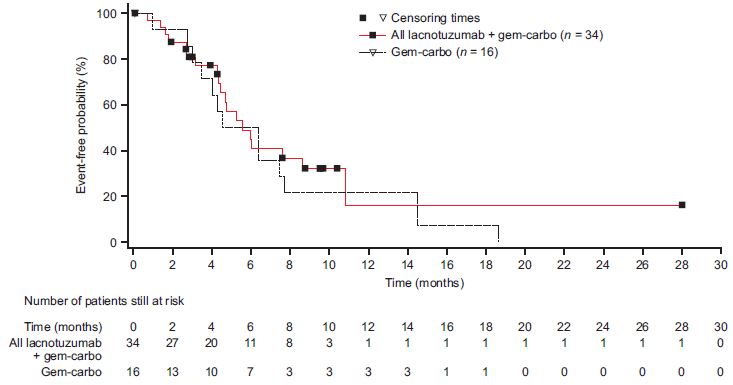
两治疗组的无进展生存期
共招募了49位患者,其中34位接受了Lacnotuzumab+吉西他滨+卡铂治疗,15位患者接受了吉西他滨+卡铂治疗。由于治疗领域的快速发展,招募面临挑战,因此招募停止,并未对主要终点进行正式假设检验。
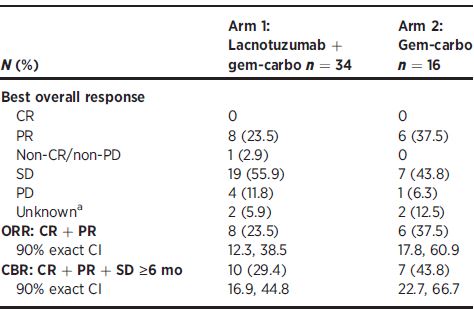
两治疗组的最佳治疗反应
联合组和吉西他滨+卡铂组的中位无进展生存期分别是5.6个月和5.5个月。两组最常见的副反应都是血液系统副反应;但是,接受Lacnotuzumab治疗的患者往往会经历更高频率的天冬氨酸氨基转移酶、丙氨酸氨基转移酶和肌酸激酶升高。
综上,Lacnotuzumab+吉西他滨+卡铂在晚期TNBC中显示出了与单用吉西他滨+卡铂相当的抗肿瘤活性,但耐受性稍差。
原始出处:
Sherko Kuemmel, Mario Campone, Delphine Loirat, et al. A Randomized Phase II Study of Anti-CSF1 Monoclonal Antibody Lacnotuzumab (MCS110) Combined with Gemcitabine and Carboplatin in Advanced Triple-Negative Breast Cancer. Clin Cancer Res December 3 2021 DOI:10.1158/1078-0432.CCR-20-3955
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阴性乳腺癌#
44
#晚期三阴性乳腺癌#
51
#铂#
38
#mAb#
39
#卡铂#
43
#三阴性#
54