BIOMATERIALS:乳腺癌治疗效果显著,纳米聚合物变革给药方式
2017-06-27 佚名 康健新视野
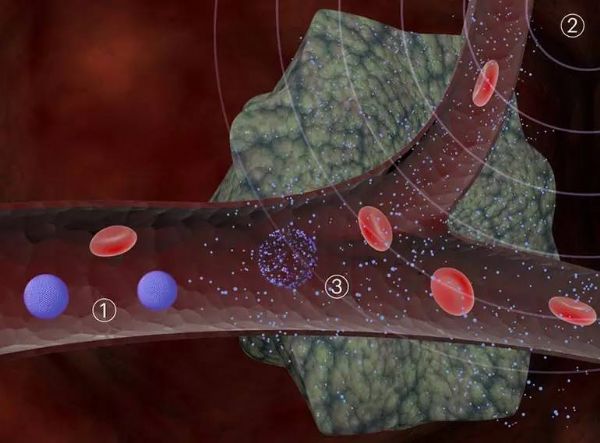
虽然都可以称为癌症,但是由于所处的组织不同,治疗方案就不能一概而论。以皮肤癌为例,位于体表,通过手术或者放疗都可以进行治疗,这对于身体内整体的健康细胞造成的损伤很低;而对于胰腺癌这种类型,癌变组织在身体的深处,只有通过血液将能够杀灭癌细胞的化疗药物带到病灶,理想状态中,肿瘤细胞萎缩依赖于药物在疾病组织的血液和淋巴管中积累的量高于正常组织,这样的方式只有通过其他的思路才能减低对健康组织的毒性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biomaterials#
30
#Bio#
40
#治疗效果#
25
#给药方式#
32
不错的,学习了,谢谢分享!
53
#聚合物#
36
很值得期待,据说很好
49