Cardiovasc Diabetol:血浆动脉粥样硬化指数与心血管疾病风险的相关性
2022-05-30 MedSci原创 MedSci原创
血浆动脉粥样硬化指数与心血管疾病风险显著相关
血浆动脉粥样硬化指数(AIP)由甘油三酯和高密度脂蛋白胆固醇组成,是评估动脉粥样硬化风险和心脏代谢健康的新指标。据报道,AIP 与 2 型糖尿病和高心血管 (CV) 疾病风险患者的主要不良心血管事件 (MACE) 的较高发生率之间存在关联。但是,只有少数研究探究了一般人群中 AIP 和心血管疾病风险之间的相关性。
该研究旨在使用来自韩国国民健康保险服务-国民健康筛查队列 (NHIS-HEALS) 的大规模人口数据集来评估血浆动脉粥样硬化指数和心血管疾病之间的关系。
研究人员从 NHIS-HEALS 中筛选了 514866 位受试者,并根据 AIP 四分位数进行分类;依次进行了单变量和多变量 Cox 比例风险回归分析,以评估 AIP 与 MACE、CV 事件和 CV 死亡率之间的相关性。
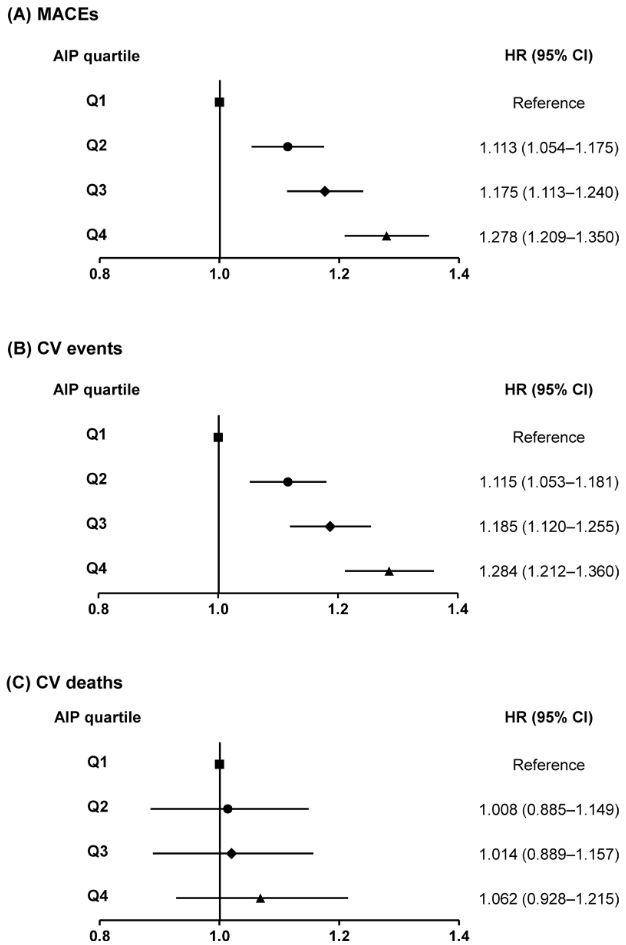
AIP 四分位数组患者MACE、CV 事件和 CV 死亡的风险比
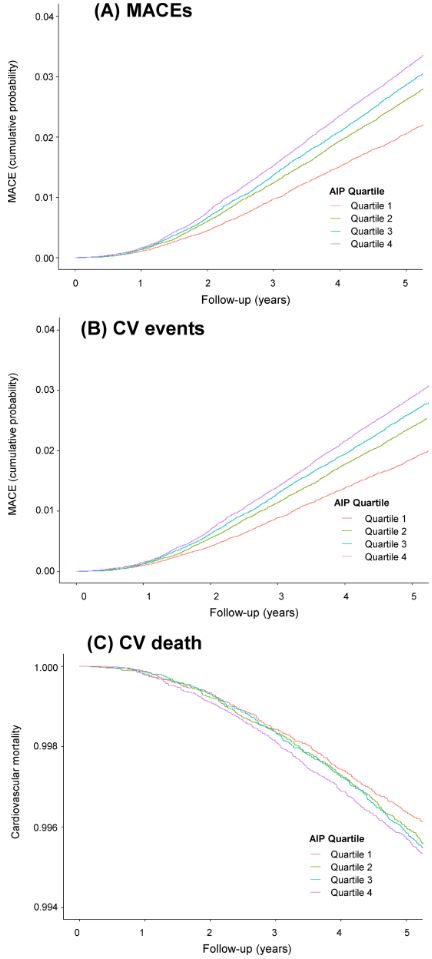
在随访期间,研究人员分别记录到了 12133、11055 和 1942 例 MACE、CV 事件和 CV 死亡事件。根据常规 CV 风险因素(包括年龄、性别、体重指数、吸烟、饮酒、体育活动、家庭收入、空腹血糖、收缩压、低密度脂蛋白胆固醇和估计的肾小球滤过率)调整的风险比(HR)随着 AIP 四分位数逐渐显著增加(与 Q1 相比,Q2、Q3 和 Q4 的 HR 分别是 1.113、1.175 和 1.278)。亚组分析显示,AIP 与 MACE 和 CV 事件的关联在糖尿病患者中尤为突出。
AIP 四分位数组患者的心血管预后和死亡率
综上所述,根据传统风险因素调整后,血浆动脉粥样硬化指数与心血管疾病风险显著相关。因此,血浆动脉粥样硬化指数可以作为一种有效的大规模筛查方法来识别高心血管事件风险的患者。
原始出处:
Kim, S.H., Cho, Y.K., Kim, YJ. et al. Association of the atherogenic index of plasma with cardiovascular risk beyond the traditional risk factors: a nationwide population-based cohort study. Cardiovasc Diabetol 21, 81 (2022). https://doi.org/10.1186/s12933-022-01522-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#粥样硬化#
47
#ASC#
0
#BET#
30
#DIA#
36
#相关性#
29
学习了
49
#疾病风险#
32
#血管疾病#
30
学习
42