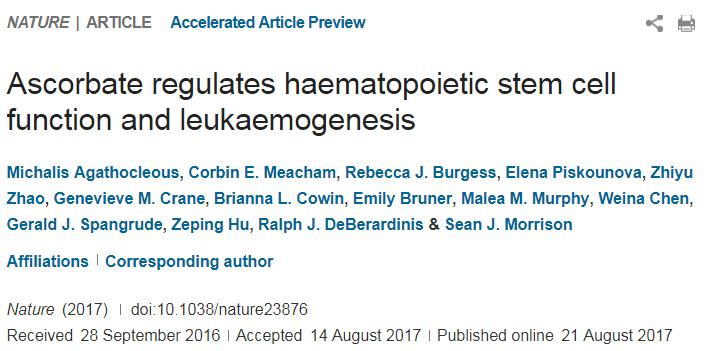
EMBO Rep:北京基因组所等揭示维生素C是潜在的肾癌分化治疗小分子
2018-07-11 佚名 北京基因组研究所
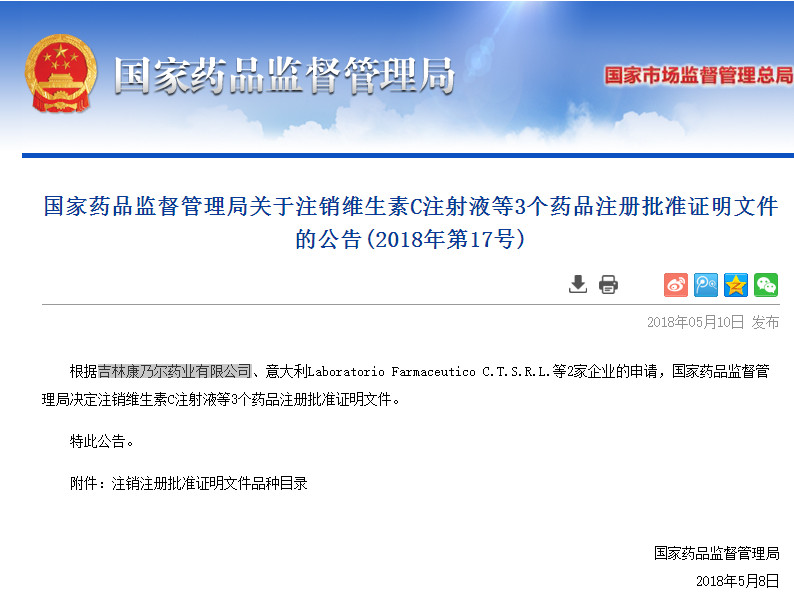
维生素C是日常生活中必不可少的营养元素,具有增强抵抗力、抗氧化及美容的功效。自从1970年诺贝尔奖获得者、生物化学家鲍林发表论文认为维生素C可以防治癌症以来,争议的声音也一路伴随,但对维生素C与肿瘤关系的研究从未停止。高剂量的维生素C虽然可以应用在肿瘤治疗中,但是其不稳定性以及高剂量带来的毒性,使得肿瘤治疗中维生素C的开发与利用停滞不前。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#小分子#
33
*
66
学习一下
64
***
62
***
79