胃癌(carcinoma of stomach)内镜-CT病例图片影像诊断分析
2022-09-02 放射沙龙 影像园
早期胃癌是指病灶局限且深度不超过粘膜下层的胃癌,无论有无局部淋巴结转移。进展期胃癌是指胃癌深度超过粘膜下层,已超过肌层者称中期,侵及浆膜或浆膜外者称晚期胃癌。
【病史临床】
男,44岁,剑突下疼痛伴呕吐半年余,加重1周。
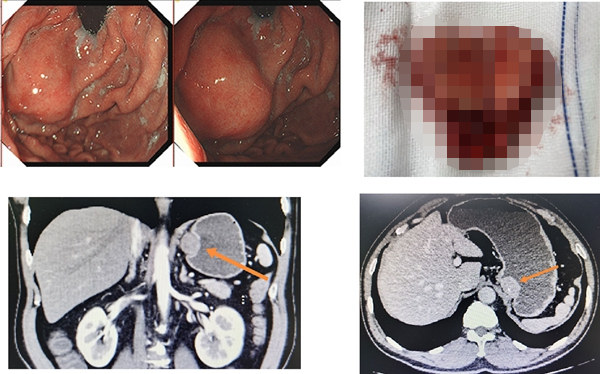
【影像图片】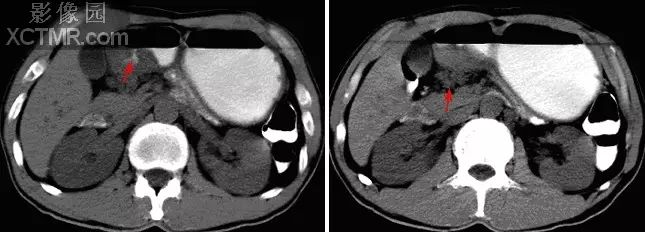 平扫
平扫
 增强
增强
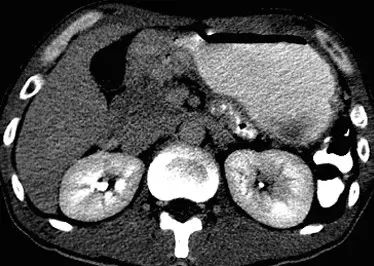
 胃镜
胃镜
【影像表现】
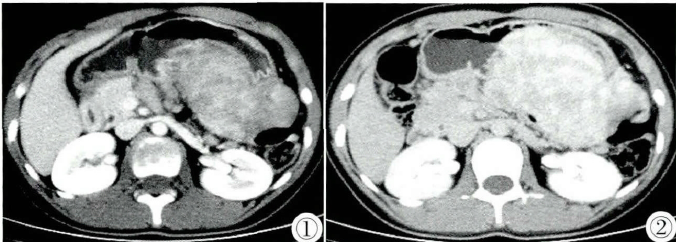
CT表现:胃窦部胃壁局限性增厚(图3),局部并可见龛影(图1箭头),增强扫描病灶明显强化。胃窦部胃小弯可见数枚肿大淋巴结(图2箭头)。胃镜所见:胃窦部类圆形占位性病变突出于胃腔内,表面可见溃疡。
【诊断】
胃癌
【鉴别诊断】
1.胃淋巴瘤 2.胃间质瘤 3.胃间质肉瘤 4.痉挛性狭窄
【讨论】
胃癌(carcinoma of stomach)是消化系统常见恶性肿瘤之一,男性多见,发病年龄在40~60岁,从发病部位上看,以胃小弯胃窦部最常见,占50%~60%,其次为贲门胃底区,胃体部及大弯侧发病率最低。临床上主要表现为上腹部隐痛不适,进而出现恶心、呕吐等。根据胃癌的进程可分为早期胃癌及进展期胃癌。早期胃癌是指病灶局限且深度不超过粘膜下层的胃癌,无论有无局部淋巴结转移。进展期胃癌是指胃癌深度超过粘膜下层,已超过肌层者称中期,侵及浆膜或浆膜外者称晚期胃癌。进展期胃癌的Borrmann分期:Ⅰ型:息肉型或蕈伞型,肿瘤呈结节状,向胃腔内隆起生长,边界较清楚,不多见。Ⅱ型:溃疡型,单个或多个溃疡,边缘隆起,形成堤坎状,边界较清楚,常见。Ⅲ型:溃疡浸润型,结节状的边缘向周围浸润,与正常粘膜无清晰的边界,最常见。Ⅳ型:弥漫浸润型,癌组织发生于粘膜表层之下,在胃壁向四周弥漫浸润扩散,同时伴有纤维组织增生,少见。
影像学诊断要点:
内镜检查:内镜检查结合粘膜活检是目前最可靠的诊断手段。应在病灶边缘与正常粘膜交界多处活检,至少活检取6块以上。内镜下对病灶进行美蓝染色(癌性病变处无着色),可以大大提高病灶的捡出率。
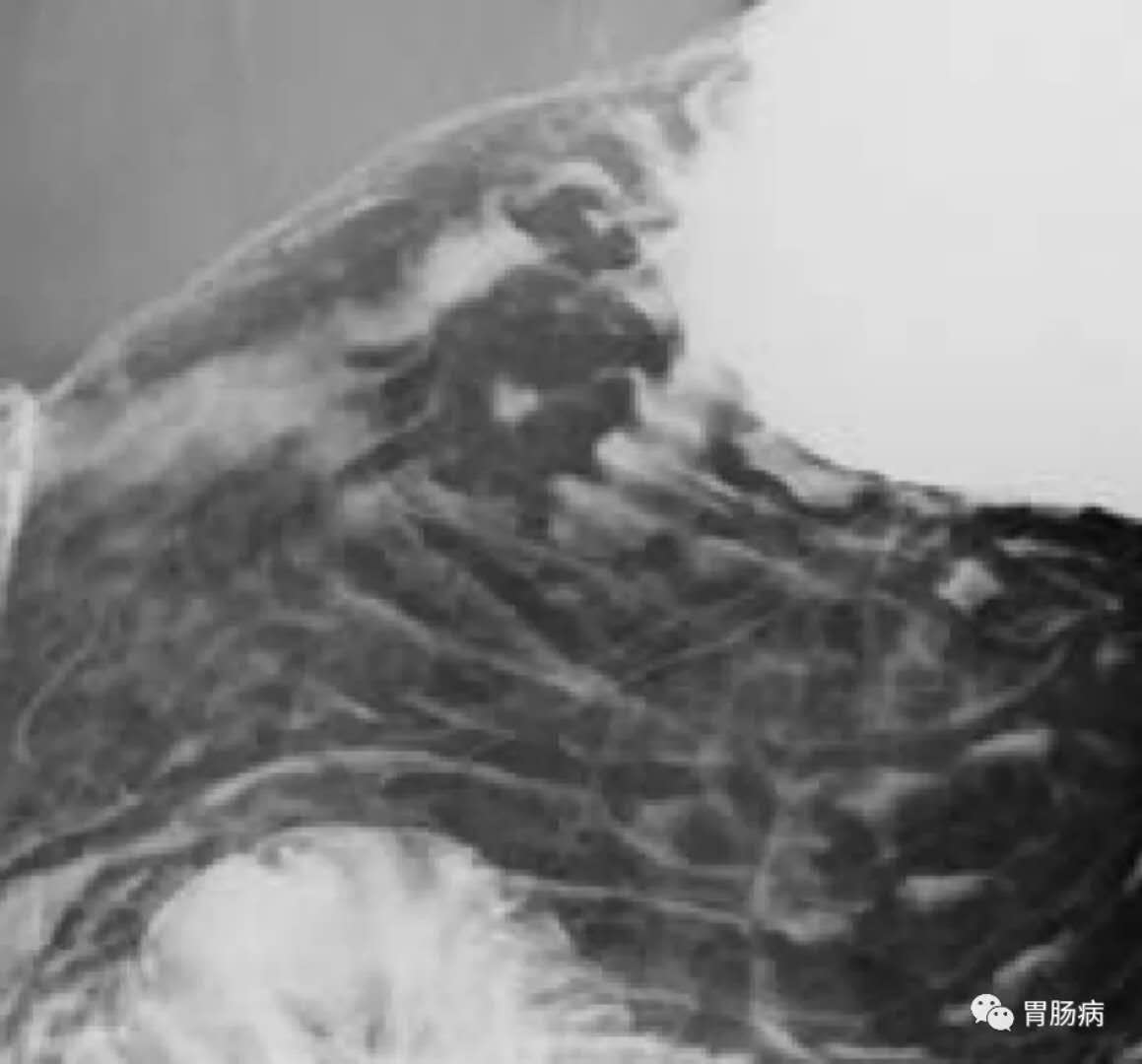
X线:早期胃癌:低张双重对比造影
(1)胃小区粘膜结构紊乱、消失
(2)切线位上可见刺突样小龛影
(3)可见颗粒状、小圆形充盈缺损,表面毛糙不平。进展期胃癌:肿瘤局部黏膜皱襞中断消失;胃轮廓毛糙不整,胃腔变形狭窄;边缘不整,凹凸不平,形成菜花状充盈缺损;恶性溃疡征象如“半月综合征”、“环堤征”、“裂隙征”,腔外龛影等;局限性胃壁僵硬、蠕动消失。
图1~3为另一病理证实为胃癌的钡餐图像:图1显示为腔内龛影 图2显示“半月综合征” 图3显示为胃壁局部充盈缺损,粘膜纠集现象。
CT检查:平扫可见不规则软组织影突向腔内,胃壁弥漫性或局限性增厚(CT图像一般把胃壁厚度>10mm视为异常,但如发现局限性增厚,即便<10mm,亦应视为异常),壁不光滑。动态CT增强上表现为突出胃黏膜皱襞之间的明显强化区,肿瘤中度或明显不均一强化,静脉期病灶均一强化。CT能准确显示肿瘤对周围器官的侵犯征象,表现为病变区胃轮廓不清,浆膜面毛糙,胃周脂肪层模糊不清或消失,病变区可见延伸向胃周的不规则条带状致密影,还可以显示病灶对周围脏器的侵犯,和腹腔淋巴结的转移情况。
MRI:中晚期胃癌MRI信号表现为T1WI呈中等或稍低信号,T2WI呈中等高信号。增强扫描病灶呈不均匀中等程度强化。其它表现类似于CT。
与胃淋巴瘤相鉴别:好发于40岁以上,好发于胃体、胃窦部。临床症状轻,胃腔缩小较胃癌少见,幽门梗阻的概率也较少。X线表现为胃内较大龛影,粘膜广泛受侵,较多息肉样或结节样表现,胃窦部多呈漏斗状狭窄为其X线特征。CT上显示胃壁弥漫性增厚,强化程度不如胃癌,且对胃周脂肪及临近器官的侵犯不如胃癌明显。胃淋巴瘤的腹内淋巴结转移较胃癌淋巴结转移数目多且体积较大。
与间质瘤相鉴别:发生于胃固有肌层的良性肿瘤,男性稍多,好发于50~60岁。X线表现为黏膜下肿瘤的特点,典型者半圆形边缘光滑的隆起,可有桥形皱襞。CT表现为发生于胃壁并向胃腔内和(或)腔外突出的肿块,边界清楚,密度均匀,胃粘膜受压变薄,但其完整性良好。增强扫描肿块内侧胃粘膜面形成连续的弧线性强化为其特征性表现。
与间质肉瘤相鉴别:临床症状明显,病程短,肿瘤生长迅速,出血、液化及坏死多见,表面常并有溃疡形成。间质肉瘤起源于胃黏膜下,且多向腔外生长。CT扫描示肿块内有地图样或裂隙性低密度区,增强后,周边强化,中心低密度区不强化。与胃癌鉴别困难。
【问题】
Ture OR False
(1)病灶位于胃窦部 对: 错
(2)病灶表现为胃壁的局限性增厚 对: 错
(3)病灶未见强化 对: 错
(4)周围淋巴结转移 对: 错
(5)肿块胃外侵犯 对: 错
正确答案: 1:√ 2:√ 3:×(病灶明显强化) 4:√ 5:√
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CT病例#
49
#MAC#
66
#CIN#
62
#Stoma#
39
#Stomach#
57
#内镜#
36
#carcinoma#
38
#影像诊断#
36