Cardiovasc Diabetol:甘油三酯-葡萄糖指数和剩余SYNTAX评分在预测接受经皮冠状动脉介入治疗的2型糖尿病患者中期主要心脏不良事件中的协同作用
2022-07-22 从医路漫漫 MedSci原创
胰岛素抵抗(IR)是T2DM的一个特征,已被证明与动脉粥样硬化性心血管疾病的发生、发展和预后显著相关。
背景:冠心病是全球范围内的首要死亡原因,2019年导致890万人死亡,占全球死亡率的16%。二型糖尿病糖尿病(T2DM)是冠心病的主要危险因素。胰岛素抵抗(IR)是T2DM的一个特征,已被证明与动脉粥样硬化性心血管疾病的发生、发展和预后显著相关。T2DM患者通常有更广泛的冠状动脉粥样硬化,心血管不良事件的发生率显著增加,冠状动脉介入治疗后的预后较差。残差句法评分(rSS)是经皮冠状动脉介入治疗(PCI)后血管重建的血管造影完整性的定量指标,已被证实为PCI后不良心血管事件的独立预测因子。尽管已经明确,T2DM患者PCI后预后更差,但IR并未作为一个变量纳入rSS模型。根据空腹血糖和甘油三酯计算的甘油三酯-葡萄糖(TyG)指数被认为是胰岛素抵抗的可靠替代指标。先前的文献表明,高TyG指数与无症状成年人冠状动脉钙化进展和狭窄增加相关,并与普通人群心血管疾病风险增加相关。此外,TyG指数在不同的队列中显示出强大的PCI后风险预测能力,包括急性ST段抬高心肌梗死患者(STEMI) ,糖尿病患者和非糖尿病非ST段抬高急性冠脉综合征患者(NSTE-ACS) ,T2DM急性冠脉综合征患者和非糖尿病冠心病患者。据我们所知,TyG指数对接受PCI的T2DM患者的预后价值尚未得到彻底研究。此外,没有相关研究关注增加TyG指数是否能提高接受PCI的T2DM患者rSS的预测能力。
目的:在本研究中,我们研究了TyG指数对接受PCI的T2DM患者不良心血管事件的预测价值,以及TyG指数与rSS联合应用的潜在增量预后价值。
方法:总共633名连续的T2DM患者接受了PCI,包括在目前的分析中。根据TyG指数的最佳分界点值或通过受试者工作特征(ROC)曲线分析确定的rSS对患者进行分层。主要终点是MACEs的综合指标,包括全因死亡、非致死性心肌梗死和意外的重复血运重建。使用卡普兰-迈耶方法计算累积曲线。多变量Cox回归用于确定MACEs的预测因子。通过ROC曲线下面积、连续净重新分类改进(NRI)和综合判别改进(IDI)来估计TyG指数结合rSS的预测值。结果:在中位数为18.83个月的随访中,99名患者发生了MACEs,在TyG指数或rSS较高的患者中更为常见。多变量Cox风险回归分析显示TyG指数和rSS都是MACEs的独立预测因子(风险比为1.8004;95%可信区间为1.2603–2.5718;P = 0.00121.0423;95%CI 1.0088–1.0769;P = 0.0129)。此外,Kaplan-Meier分析表明,TyG指数和rSS与MACEs风险增加显著相关(log rank,均P < 0.01)。将rSS和TyG指数添加到基线风险模型中对MACE的预测值有增量效应(C统计值从0.660增加到0.732;IDI 0.018;NRI 0.274;均P < 0.01)。
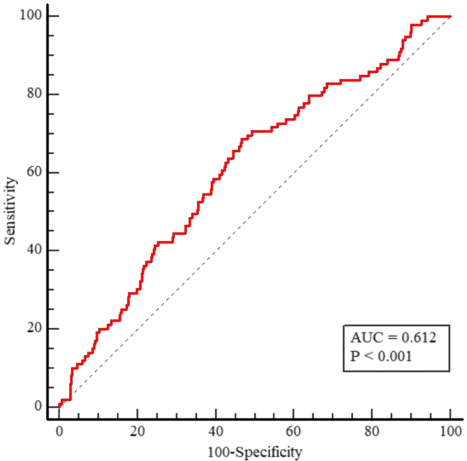
图1 MACEs TyG指数的ROC曲线分析。甘油三酯-葡萄糖(TyG)指数的受试者工作特征(ROC)曲线作为预测T2DM患者PCI术后MACEs的标志。预测T2DM患者PCI术后18个月内发生MACEs的TyG指数的ROC曲线下面积(AUC)为0.612(95% CI 0.573-0.650;P < 0.001)。T2DM2型糖尿病,MACE主要不良心脏事件,PCI经皮冠状动脉介入治疗
表1根据TyG指数的最佳临界值得出的患者基线特征
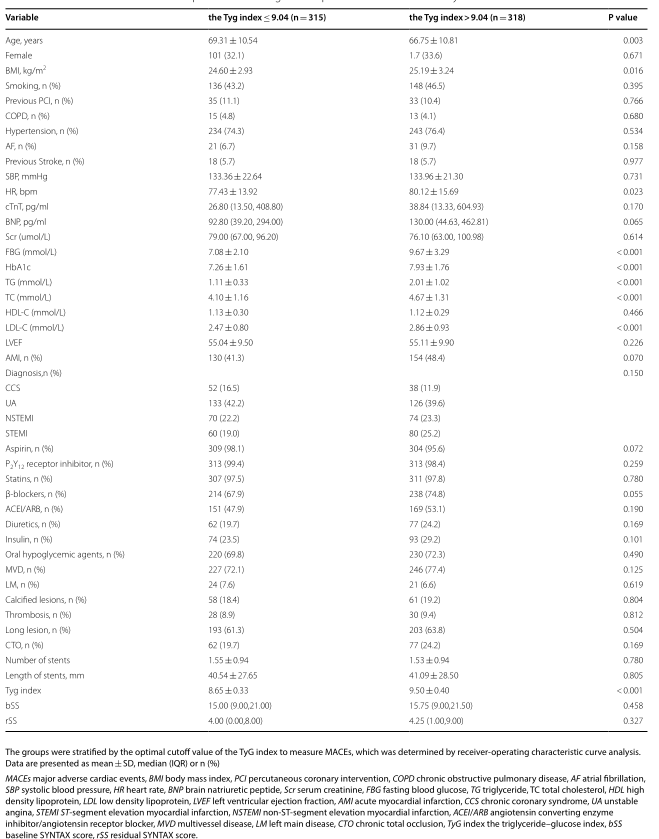
表2两组中期不良预后的比较


图2 根据TyG指数的最佳临界值,终点事件的累积发生率。基于TyG指数的2个研究组间主要终点(A)、全因死亡(B)、心血管死亡(C)、非致死性心肌梗死(D)、非计划重复血运重建(E)和非致死性卒中(F)发生率的Kaplan-Meier曲线。根据受试者操作特征曲线分析确定的TyG指数的最佳临界值对各组进行分层。TyG表示甘油三酯-葡萄糖
表3预测PCI术后MACEs的单变量和多变量Cox回归分析
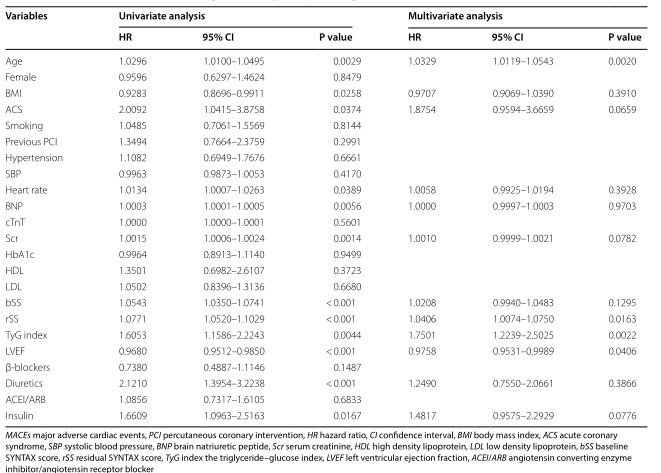

图3 MACEs rSS的ROC曲线分析。剩余语法评分(rSS)的受试者工作特征(ROC)曲线作为预测T2DM患者PCI术后MACEs的标志。rSS预测T2DM患者PCI术后18个月内发生MACEs的ROC曲线下面积(AUC)为0.673 (95% CI为0.635-0.710,P < 0.001)。二型糖尿病T2DM;MACE,主要心脏不良事件;PCI 经皮冠状动脉介入治疗
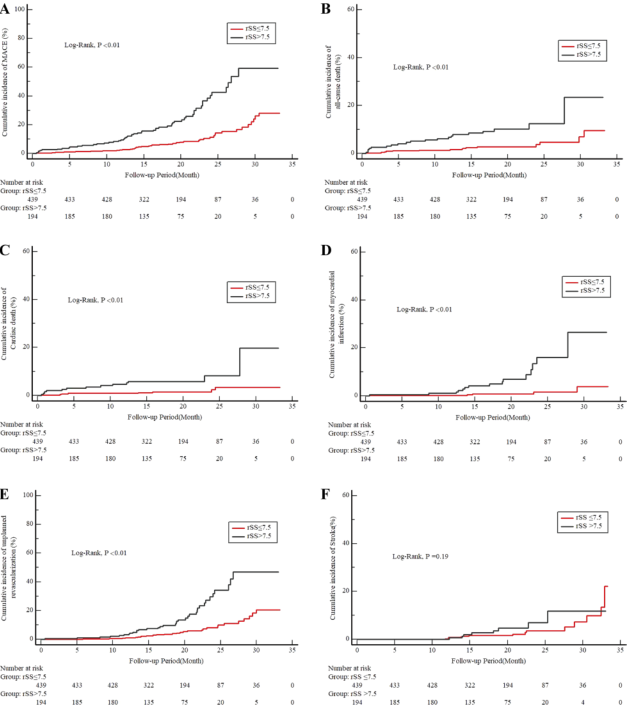
图4根据rSS的最佳临界值,终点事件的累积发生率。基于rSS的2个研究组间主要终点(A)、全因死亡(B)、心血管死亡(C)、非致死性心肌梗死(D)、非计划重复血运重建(E)和非致死性卒中(F)发生率的Kaplan-Meier曲线。根据受试者操作特征曲线分析确定的rSS最佳临界值对各组进行分层。rSS指示剩余的语法分数
结论:TyG指数独立于已知的心血管危险因素预测T2DM患者PCI术后中期MACE。通过TyG指数调整rSS进一步提高了接受PCI的T2DM患者MACEs的预测能力。
原文出处:Xiong S, Chen Q, Zhang Z,et al.A synergistic effect of the triglyceride-glucose index and the residual SYNTAX score on the prediction of intermediate-term major adverse cardiac events in patients with type 2 diabetes mellitus undergoing percutaneous coronary intervention.Cardiovasc Diabetol 2022 Jun 24;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#冠状动脉介入治疗#
36
#SYNTAX评分#
31
#ASC#
26
#心脏不良事件#
38
#DIA#
38
#BET#
30
#经皮冠状动脉介入治疗#
42
#2型糖尿病患者#
39
#糖尿病患者#
34