ICER最终报告:Elagolix对子宫内膜异位症的长期安全性和有效性
2018-08-05 MedSci MedSci原创
临床和经济评论研究所(ICER)近日发布了一份关于elagolix(Orilissa,AbbVie)的最终证据报告,近期,elagolix已被FDA批准用于治疗与子宫内膜异位症相关的中度至重度疼痛。
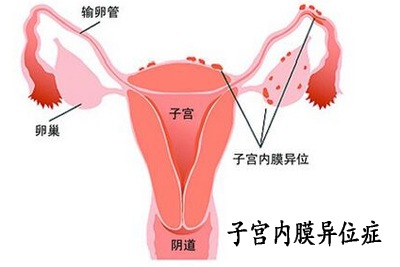
临床和经济评论研究所(ICER)近日发布了一份关于elagolix(Orilissa,AbbVie)的最终证据报告,近期,elagolix已被FDA批准用于治疗与子宫内膜异位症相关的中度至重度疼痛。子宫内膜异位症(endometriosis)是指内膜细胞种植在子宫内膜以外的位置而形成的一种女性常见妇科疾病。内膜细胞本该生长在子宫腔内,但由于子宫腔通过输卵管与盆腔相通,因此使得内膜细胞可经由输卵管进入盆腔异位生长。本病多发生于生育年龄的女性,青春期前不发病,绝经后异位病灶可逐渐萎缩退化。
ICER的报告己经在2018年7月的新英格兰比较效率公共咨询委员会(新英格兰CEPAC)公开会议上进行了审核,该委员会是ICER的三个独立证据评估委员会之一。在审议过程中,委员会成员讨论了关于子宫内膜异位症对妇女生活质量的重大影响,elagolix作为口服药物的可用性的优势,以及该药物的其他独特特征。他们还注意到治疗的长期副作用和临床益处的不确定性,因为在临床试验中,elagolix的使用限于6-12个月。
原始出处:
http://www.firstwordpharma.com/node/1583057?tsid=4#axzz5NCMJrdAy
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Elagolix#
39
#安全性和有效性#
22
#ICER#
30
#子宫内膜异位#
29
#内膜#
27
#长期安全性#
45