J Arthroplasty:全髋关节置换术后可改善患者功能
2014-11-12 虎群盛 丁香园
肥胖人群在发达国家人口中的比例在不断增加,因此,下肢骨性关节炎的发病率也在持续上升,据英格兰和威尔士国家关节登记中心的数据,在2011年全髋关节置换中身高体重指数超过30kg/m2的肥胖患者已经占到了38%,而这一比例在2003年还不到30%。身高体重指数升高会导致关节置换手术难度增加,手术时间延长,术后并发症的发生率也会增加。 患者自我报告结局估量Patient reported
肥胖人群在发达国家人口中的比例在不断增加,因此,下肢骨性关节炎的发病率也在持续上升,据英格兰和威尔士国家关节登记中心的数据,在2011年全髋关节置换中身高体重指数超过30kg/m2的肥胖患者已经占到了38%,而这一比例在2003年还不到30%。身高体重指数升高会导致关节置换手术难度增加,手术时间延长,术后并发症的发生率也会增加。
患者自我报告结局估量Patient reported outcome measures (PROM) 是以患者自身描述受益情况的方法,是传统临床评估关节置换术后成功与否方法的补充。自从2008年起在英格兰和威尔士的国家医疗服务中心卫生部就开始收集全髋关节置换术后患者的自我报告结局估量,该体系包括患者的基本健康情况、特定的关节评分以及自我报告的并发症等数据。
英国的Simon S. Jameson收集国家关节登记中心以及自我报告结局估量的数据,研究发现:无论患者的身高体重指数如何,在全髋关节置换术后均可获得很大程度的功能改善,但是肥胖患者不仅恢复情况明显较差,而且具有较高的并发症发生率。其研究结果发表在2014年10月的The Journal of Arthroplasty杂志上。
为避免不同假体类型对患者功能恢复等方面的影响,作者选用那些最常使用的关节假体的患者资料,排除非骨性关节炎的患者以及资料不全、极度消瘦或肥胖的患者(<19kg/m2或>65kg/m2)。共有5535例患者符合纳入标准和排除标准被纳入研究,其中2656例患者使用骨水泥型关节假体,2879例使用非骨水泥型假体。
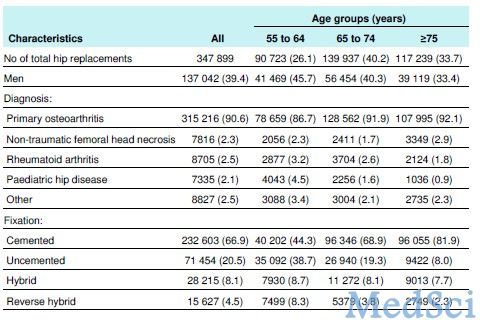
按照身高体重指数进行分组,在骨水泥型假体患者中,正常和轻度超重(19.0-29.9kg/m2)的患者有1640例,作为参照组,占61.7%;肥胖(30.0-34.9kg/m2)的患者有695例,为肥胖组I,占26.2%;严重肥胖(35.0kg/m2)的患者有321例,为肥胖组II/III,占12.1%。肥胖患者多见于女性、年轻患者,常常合并糖尿病和高血压疾病。虽然肥胖与非肥胖患者在其他合并疾病方面并无显著差异,但是肥胖患者术前的剑桥髋关节评分、欧洲五维生活质量量表、欧洲五维生活质量可视化评分等方面的情况更差。患者的具体情况见表1。
表1 :骨水泥假体患者根据身高体重指数分组后基本情况以及手术、恢复情况

在非骨水泥型假体患者中,正常和轻度超重(19.0-29.9kg/m2)的患者有1738例,占60.4%;肥胖(30.0-34.9kg/m2)的患者有713例,为肥胖组I,占24.8%;严重肥胖(35.0kg/m2)的患者有428例,为肥胖组II/III,占14.9%。和骨水泥型假体组患者相似,肥胖患者相对年龄较轻、ASA评分更高,术前的剑桥髋关节评分、欧洲五维生活质量量表、欧洲五维生活质量可视化评分等方面的情况更差。肥胖与非肥胖患者在男女比例、高血压、糖尿病、抑郁症方面存在显著差别。具体情况详见表2。
表2 骨水泥假体患者根据身高体重指数分组后基本情况以及手术、恢复情况

骨水泥组和非骨水泥组大部分的手术是在脊髓神经阻滞麻醉下侧卧位通过后侧入路进行的,脊髓神经阻滞麻醉的比例分别为78.8%(1792例)和80.4%(1923例),侧卧位的比例分别占79.1%(2102例)和78.4%(2256例)。后侧入路所占的比例分别为55.4%(1471例)和63.6%(1830例)。为避免静脉血栓性疾病,大多数的患者接受了低分子肝素和机械性预防治疗,低分子肝素的使用比例分别为53.6%(1218例)和66.2%(1593例),机械性预防的比例占80.3%(2133例)和89.9%(2636例)。
无论患者的身高体重指数如何,所有患者在髋关节置换术后其下肢功能较术前均获得显著改善,单一因素回归分析未能发现不同身高体重指数组患者在剑桥髋关节评分方面存在显著差异,但是将混杂因素排除校正后的的多元回归分析则显示肥胖患者的功能恢复情况明显较差。
在欧洲五维生活质量评分方面,单一因素回归分析未能发现骨水泥组患者不同身高体重指数组患者在术后改善方面存在差别。但是将危险混杂因素进行校正后,肥胖组患者的评分改善方面要比参照组差,但并未达到显著意义的水平。
和骨水泥组患者相比,非骨水泥组的情况又有所差别,单一因素回归分析显示虽然未能达到显著差异水平,但是肥胖组II/III的功能改善情况要要优于参照组。将危险混杂因素进行校正后,肥胖组II/III的功能改善情况要要明显差于参照组,并且具有统计学意义。
将骨水泥假体组患者排除混杂因素校正后进行统计分析,和参照组相比,肥胖II/III组患者术后并发症要明显较高,例如伤口并发症、再次入院率、二次手术率。肥胖I组患者的并发症明显减少,只有伤口并发症的发生率提高了1%。不同体重指数组患者之间出血风险相似。
而在非骨水泥组患者中,将混杂因素排除后,肥胖II/III组患者的伤口并发症发生率要明显高于参照组。但是各组患者在出血并发症、再次入院率、二次手术率等方面并无显著差异。
因此作者认为:髋关节置换手术可以有效的治疗老年骨性关节炎,无论患者是否肥胖,术后均可获得一定程度的功能改善。但是肥胖患者的功能恢复会比较差,更容易出现术后并发症。
原始出处
Jameson SS1, Mason JM2, Baker PN3, Elson DW4, Deehan DJ4, Reed MR5.The impact of body mass index on patient reported outcome measures(PROMs)and complications following primary hip arthroplasty.J Arthroplasty. 2014 Oct;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#全髋关节#
45
#关节置换术#
45
#置换#
42
#AST#
39
#ART#
41
#置换术#
32