Cell Host & Microbe:毛囊滋养的不只是发根,更能调节免疫系统
2017-03-27 Leo.C MedSci原创
Ccl20- Ccr6信号通路是诱导T细胞迁移到皮肤,并在毛囊与细菌接触,从而吸引更多的T细胞迁移,并且产生Treg细胞的重要机制
调节型T(regulatory T, Treg)细胞在免疫系统中起到抑制机体过度免疫的作用,从而达到免疫系统的平衡抑制过免疫疾病的发生。尤其是在一些与外界细菌长期接触的局部组织,比如肠道与皮肤,Treg细胞的数量与功能对于抑制炎症疾病比如肠炎和过敏性皮肤炎有直接的作用。因此,从新生儿刚出生开始接触细菌的同时,Treg细胞在开始在这些组织中积累。与细菌的接触直接决定了Treg细胞的产生。此前的报导证明,在无菌环境下出生的实验鼠的Treg细胞数量要远远低于在有菌情况下出生的实验鼠。
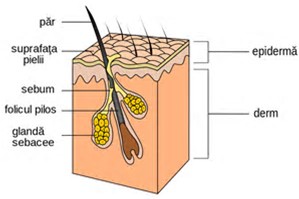
为了耐受外界细菌的刺激产生Treg细胞,组织器官发展出特定的结构促进免疫细胞与外界细菌的接触。比如在肠道中的各种淋巴腺,包括潘氏淋巴腺 (peyer’s patches)和肠道黏膜下的淋巴结。相反的,在皮肤上没有这样的淋巴组织,那么皮肤的免疫细胞是怎样与外界细菌的接触并且产生Treg细胞呢?
在最近一期的Cell Host and Microbe杂志上,Tiffany C. Scharschmidt 及其同事发现皮肤上的毛囊是免疫细胞与外界细菌的接触及产生Treg细胞主要场所。研究团队首先通过比较无毛囊与毛发正常的老鼠发现,Treg细胞有偏好性的主要聚集在毛囊区域。其次通过比较在无菌环境和有菌环境下出生的实验鼠发现,无菌环境下出生的实验鼠的毛囊内Treg细胞数量大大减少。新生鼠的Treg细胞在出生后的第六天开始大量积累并且在第十三天达到平台期,通过比较新生鼠第十三天与第六天的皮肤基因的表达,研究者发现负责细胞移动的趋化因子Ccl20和Ccl22在第十三天的皮肤组织中有更高的表达,并且在有细菌接触的情况下表达更高。同时在从十三天大的新生鼠皮肤上分离的Treg细胞上检测到了更高的Ccr6基因的表达。Ccr6基因是趋化因子Ccl20的受体,因此实验组推测新生鼠的皮肤可能通过分泌更多的趋化因子Ccl20从而招募更多的表达Ccr6受体的Treg细胞。并且以上基因在皮肤接触细菌的情况下,表达量更高。
除了在皮肤组织的Treg细胞有高表达的Ccr6受体以外,在产生T细胞的胸腺里也有少量部分的T细胞表达Ccr6受体。体外培养这些来自胸腺的T细胞,并且给予趋化因子Ccl20,发现这些细胞的迁移率上升。在Ccr6敲除的实验鼠上移植正常的带有Ccr6的T细胞,发现大部分迁移到皮肤的T细胞是来自移植的带有Ccr6的T细胞。从而证明Ccl20- Ccr6信号通路是诱导T细胞迁移到皮肤,并在毛囊与细菌接触,从而吸引更多的T细胞迁移,并且产生Treg细胞的重要机制。
原始出处:
Tiffany C. Scharschmidt, Kimberly S. Vasquez, Mariela L. Pauli et al. Commensal Microbes and Hair Follicle Morphogenesis Coordinately Drive Treg Migration into Neonatal Skin. Cell Host & Microbe Available online 23 March 2017 http://dx.doi.org/10.1016/j.chom.2017.03.001
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
22
#CEL#
22
#Micro#
35
#CRO#
18
#毛囊#
29