NEJM:FFR和血管造影指导下的多支血管PCI治疗心肌梗死比较(FLOWER-MI研究)
2021-07-25 网络 网络
2021年,中国冠脉介入治疗“大踏步”步入生理功能学评估的大时代,不管是传统的FFR(包括FFR压力微导管),还是算法衍生出来的QFR、caFFR等,都在临床上积极地开展着推广
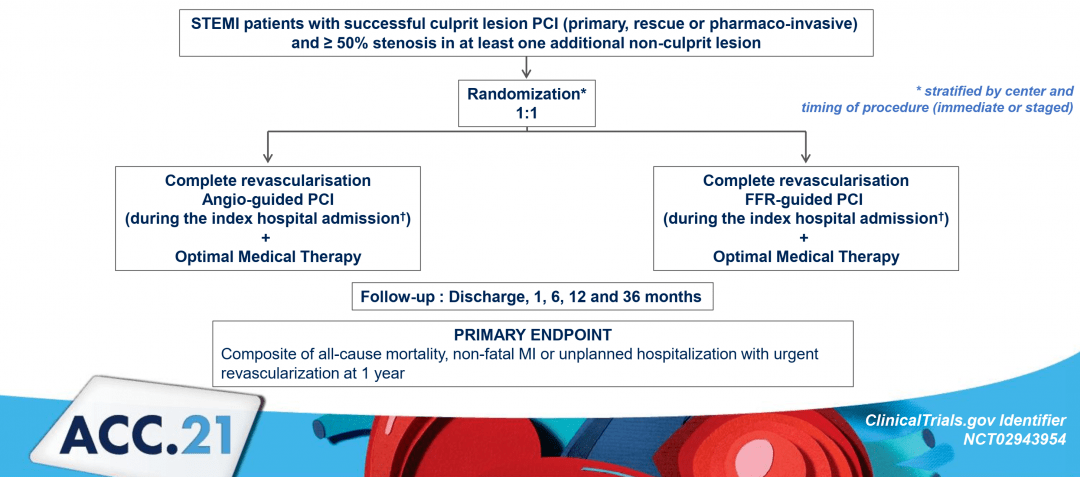
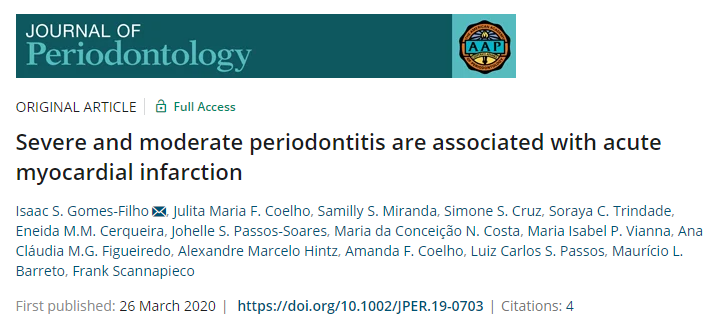
2021年,中国冠脉介入治疗“大踏步”步入生理功能学评估的大时代,不管是传统的FFR(包括FFR压力微导管),还是算法衍生出来的QFR、caFFR等,都在临床上积极地开展着推广,并开启了冠心病“无创或无压力导丝”功能学评估指导介入治疗的元年。 但是这么多“精准”工具涌现出来后,术者们又该怎么选用呢?无论如何,相信都需要用大量研究数据来支持其临床的广适性。 对于稳定性心绞痛来说,FFR无疑已经成为指导PCI的金标准,而对于ACS患者来说,FFR指导尚不明朗且有很远的路要走。 特别是对于合并多支血管病变的急性ST段抬高型心肌梗死(STEMI)患者来说,在处理完罪犯血管后FFR或单纯造影指导完全血运重建,谁能获得更好临床预后呢? FLOWER-MI研究结果给予了答案! 尽管目前的指南推荐血流储备分数(FFR)来识别稳定患者在缺乏缺血证据时的血流动力学相关冠状动脉病变(罪犯病变,I级,证据水平:A),目前尚未有发表的研究来评价ST段抬高型心肌梗死(STEMI)合并多支血管病变(MVD)患者接受FFR指导下的行经皮冠状动脉介入治疗(PCI)的有效性。 本研究的主要终点是确定在STEMI合并MVD
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#FFR#和#血管造影##心肌梗死##PCI#
96
#PCI治疗#
58
#多支血管PCI#
42
#多支血管#
46
#造影#
39
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
61
感谢分享
66