盘点:近期冠状动脉疾病重大研究进展一览
2016-12-03 MedSci MedSci原创
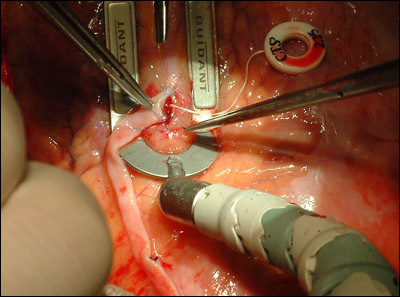
我国冠心病发病呈逐年增加态势,而经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)是治疗冠心病的主要措施。近20年来,冠状动脉血流储备分数(fractional flow reserve,FFR)逐渐成为公认的有创病变功能学评价指标,以FFR指导的治疗策略被证实安全、经济,并能改善患者的预后。本文梅斯医学小编就近期冠状动脉疾病重大研究进展汇总,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#重大研究#
34
#冠状动脉疾病#
32
#研究进展#
28
总结的咨询挺好
63
这种方式很好
50
很喜欢这种总结式的资讯,简明扼要
49