Nature:揭示出增加癌细胞抵抗免疫攻击的PD-L1基因变异
2016-06-01 生物谷 生物谷
在一项新的研究中,来自日本多家研究机构的研究人员针对成人T细胞白血病/淋巴瘤病例进行测序研究,结果发现一些癌细胞中的一些增加PD-L1蛋白产生的基因变异,这些基因变异增加癌细胞抵抗免疫系统攻击。相关研究结果近期发表在Nature期刊上,论文标题为“Aberrant PD-L1 expression through 3′-UTR disruption in multiple cancer

在一项新的研究中,来自日本多家研究机构的研究人员针对成人T细胞白血病/淋巴瘤病例进行测序研究,结果发现一些癌细胞中的一些增加PD-L1蛋白产生的基因变异,这些基因变异增加癌细胞抵抗免疫系统攻击。相关研究结果近期发表在Nature期刊上,论文标题为“Aberrant PD-L1 expression through 3′-UTR disruption in multiple cancers”。这些基因变异有可能作为癌症患者的识别性标志物。
之前的研究已证实癌细胞中的PD-L1蛋白表达增加会导致它们抵抗人免疫系统攻击的能力增强---T细胞表面上的PD-1受体与PD-L1结合,导致T细胞不再作出反应,从而阻止它们攻击肿瘤。在这项新的研究中,研究人员对一种特定类型的癌细胞进行基因分析以便更多地了解参与导致PD-L1表达增加的遗传过程。
研究人员对49名成人白血病或淋巴瘤患者的样品进行全基因组测序,特地寻找可能解释PD-L1表达增加的基因变异。通过这样做,他们在其中的13种样品(代表着测试的这些样品的27%)中发现诸如重复、倒位和易位之类的变异存在于第9号染色体的某一部分上,而之前的研究所发现的是负责PD-L1表达的基因组片段。他们报道这些变异似乎切掉这个蛋白编码基因的3’非编码区,而且在一些情形下,导致这个基因的开放阅读框重排,从而允许更多的PD-L1蛋白表达。
为了更深一步开展研究,研究人员随后对来自33种不同类型癌症患者的1万多份样品进行基因分析,寻找相同类型的基因变异。他们在包括8%的某些淋巴瘤患者和2%的某些类型胃癌在内的多种不同类型癌症中发现这些相同的基因变异。
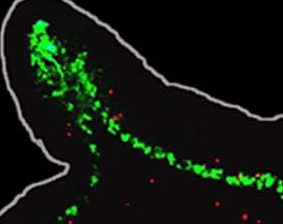
研究人员接下来在模式小鼠体内利用CRISPR/Cas9进行一些基因编辑从而破坏这些基因变异带来的影响,结果发现这样做会阻止PD-L1表达增加,并且提供更多证据证实这种增加的PD-L1表达为癌细胞免受免疫攻击提供保护。
原始出处:
Keisuke Kataoka, Yuichi Shiraishi el at Aberrant PD-L1 expression through 3′-UTR disruption in multiple cancers doi:10.1038/nature18294 Nature 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
25
#癌细胞#
32
#PD-L1#
32
#基因变异#
31
#变异#
25