大盘点| 常见静脉用抗高血压药物
2016-07-28 寇威 医学界临床药学频道
一、常见静脉用抗高血压药物二、详细讲解►硝普钠1)作用机制:动脉和静脉扩张剂。2)给药剂量:静脉滴注,从0.5 µg/kg/min开始,维持剂量3 µg/kg/min,极量10 µg/kg/min,总量3.5 mg/kg。3)起效时间:即刻。4)持续时间:1-10min。5)不良反应:轻微。主要有:a、眩晕,肌颤,出汗,心动过速等;b、硫氰酸盐超量或中毒;c、氰化物中毒;d、光敏感、高铁血红蛋
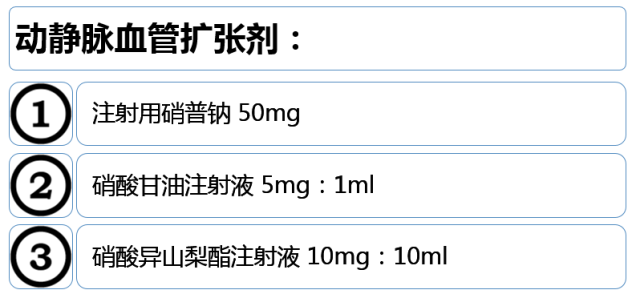
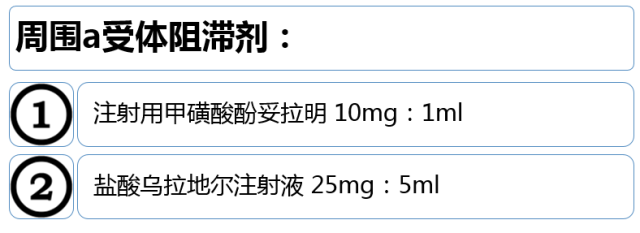
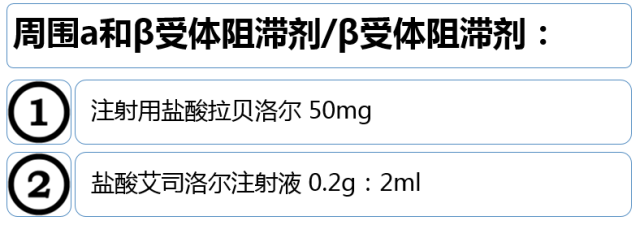
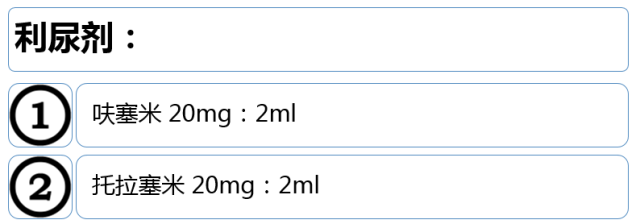
一、常见静脉用抗高血压药物

二、详细讲解
►硝普钠
1)作用机制:动脉和静脉扩张剂。
2)给药剂量:静脉滴注,从0.5 µg/kg/min开始,维持剂量3 µg/kg/min,极量10 µg/kg/min,总量3.5 mg/kg。
3)起效时间:即刻。
4)持续时间:1-10min。
5)不良反应:轻微。主要有:
a、眩晕,肌颤,出汗,心动过速等;
b、硫氰酸盐超量或中毒;
c、氰化物中毒;
d、光敏感、高铁血红蛋白血症(罕见)。
6)适应症:大多数高血压急症,尤其合并急性左心衰患者。
7)禁忌症:代偿性高血压(如动静脉分流或主动脉缩窄)。
8)注意事项:
a、潜在的毒性作用,小儿、孕妇慎用;
b、增加颅内压,高血压脑病及脑卒中病人应慎用;
c、冠心病患者有“冠脉窃血”作用;
d、甲状腺功能不全者(代谢产物硫氰酸盐抑制碘摄取)、肺功能不全(加重低氧血症)、肝肾功能不全患者慎用(氰化物浓度<3umol/ml);
e、不可与其他药物配伍,滴注需避光,配置后24h内使用。
►硝酸甘油或硝酸异山梨酯
1)作用机制:动脉和静脉扩张剂(剂量依赖)。
2)给药途径及剂量:静脉滴注,5-100 µg/min,合并肺水肿极量可至200 µg/min(硝酸甘油)。1-10 mg/h(硝酸异山梨酯)。
3)起效时间:2-5min。
4)持续时间:5-10min。
5)不良反应:头痛,皮肤潮红,恶心,呕吐,心动过速,高铁血红蛋白血症。
6)适应症:合并急性肺水肿及急性冠脉综合征的高血压急症(无冠脉窃血作用),不常规用于其他高血压急症 。
7)禁忌症:颅内高压、青光眼、严重贫血、肥厚性梗阻性心肌病、重度主动脉瓣和二尖瓣狭窄、合并使用5-磷酸二酯酶抑制剂、脑出血或头颅外伤等。
8)注意事项:
a、连续给药易致耐药;
b、个体差异明显,需密切监测血压。
►尼卡地平
1)作用机制:中小动脉扩张剂,静脉作用小;高度血管选择性(血管平滑肌:心肌=30000:1 )(椎动脉、冠状动脉、末梢小动脉等),无明显负性肌力作用,改善心脑器官血流量,保护缺血心肌;中度利尿作用。
2)给药途径及剂量:静脉滴注,从0.5 µg/kg/min开始,可逐步调量至6 µg/kg/min,特殊情况可至10-30 µg/kg/min。
3)起效时间:5~10min。
4)持续时间:1~4h。
5)不良反应:头痛,心动过速,恶心,呕吐,面部潮红,静脉炎,转氨酶升高等。
6)适应症:手术时异常高血压的短期急救处理;高血压急症,特别是伴基底动脉供血不足者、冠脉供血不足或二尖瓣关闭不全及末梢阻力和肺动脉压中度升高的患者。
7)禁忌症:重度主动脉狭窄,颅内出血尚未完全止血,脑卒中急性期颅内压增高者。
8)注意事项:口服序贯治疗,应在静脉给药停止前至少1h给予口服。
►尼莫地平
1)解除脑动脉血管痉挛作用强。
2)通过血脑屏障。
3)降压作用弱。
4)适用于合并脑血管疾病患者。
5)严重肝功能损害及脑水肿或颅内压明显升高者慎用。
►地尔硫卓
1)作用机制:舒张血管平滑肌、扩张冠脉;降低窦房结、房室结自律性及传导性,控制室上性心律失常。
2)给药剂量:静脉输注,5-15 µg/kg/min。
3)不良反应:心动过缓、浮肿、头痛、皮疹等。
4)适应症:特别是高血压合并冠心病、肥厚性心肌病、流出道狭窄者。
5)禁忌症:病态窦房结综合征、II度以上房室传导阻滞、严重充血性心力衰竭、严重心肌病患者。
6)注意事项:对心脏有抑制作用,不宜长期静脉用药。
►酚妥拉明
1)作用机制:α受体阻滞剂。
2)给药途径及剂量:首剂5~10mg缓慢静脉推注,20-30min重复给药,或0.5-1mg/min静脉滴注。
3)起效时间:即刻。
4)持续时间:10-30min。
5)不良反应:颜面潮红,头痛,心动过速,快速性心律失常,体位性低血压等。
6)适应症:适用于嗜铬细胞瘤引起的高血压危象。
7)禁忌症:严重动脉粥样硬化、肾功能不全、胃十二指肠溃疡、急性冠脉综合征患者以及过敏者。
►乌拉地尔
1)适应症:大多数高血压急症,尤其伴高血压脑病、急性左心衰竭、主动脉夹层患者,对嗜铬细胞瘤引起的高血压危象有特效。
2)禁忌症:主动脉峡部狭窄或动静脉分流患者。
3)注意事项:患者取卧位,疗程一般不超过7天。
►拉贝洛尔
1)作用机制:非选择α和β受体阻滞剂(1:7)(β受体阻滞剂作用约为普奈洛尔的40%,无明显心肌抑制作用,a受体阻滞作用约为10-15%酚妥拉明)。
2)给药途径及剂量:25-50mg缓慢静脉推注,15min重复,极量200mg,或者1-4mg/min静脉滴注。
3)起效时间:5~10 min。
4)持续时间:3~6小时。
5)不良反应:直立性低血压、恶心,头皮麻刺感或喉头发热,头晕,支气管痉挛,心动过缓,传导阻滞等。
6)适应症:大多数高血压危象,特别适用于妊娠、伴肾功能减退者;也可用于嗜铬细胞瘤引起的高血压危象(相当10-15%酚妥拉明)。
7)禁忌症:重度或急性心力衰竭、支气管哮喘、II~III度房室传导阻滞、窦性心动过缓的患者。
►艾司洛尔
1)作用机制:极短效选择性β1受体阻滞剂(33:1)。
2)给药途径及剂量:1mg/kg,30s内静脉注射,继之以0.15mg/kg/min静脉滴注,最大维持量0.3mg/kg/min。
3)起效时间:1~2min。
4)持续时间:10~20min。
5)不良反应:轻,一过性,低血压、恶心、眩晕、出汗等。
6)适应症:除心力衰竭、肺水肿外的大多数高血压危象,尤其是围手术期包括手术麻醉过程中的血压控制。
7)禁忌症:支气管哮喘、严重慢性阻塞性肺病、窦性心动过缓、II~III度房室传导阻滞、难治性心力衰竭、心源性休克及对本品过敏者。
8)注意事项:
a、高浓度给药(>10mg/ml),易至静脉炎;
b、主要通过红细胞胞质中的酯酶代谢,故不影响肝肾功能。
►利尿剂
1)作用机制:促进水和电解质排泄和扩张血管。
2)适应症:仅用于继发充血或容量超负荷的急性心力衰竭或肾衰竭患者患者。
3)首选袢利尿剂:呋塞米20-40mg,托拉塞米10-20mg,静推。
4)不良反应:电解质紊乱 。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗高血压药#
31
#抗高血压#
30
#静脉#
33
#抗高血压药物#
33
继续学习
55
继续关注
53