JAMA Neurol:颈动脉支架置入术风险与获益
2015-01-23 MedSci MedSci原创
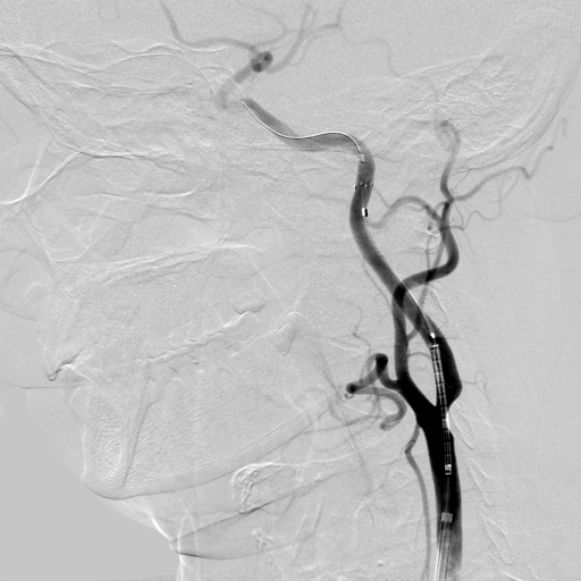
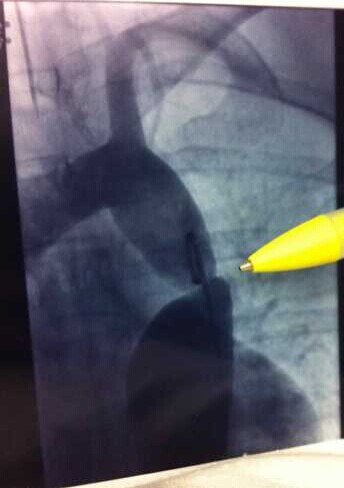
一项新的研究提出,患者接受颈动脉支架置入术(carotid artery stenting,CAS)2年后的死亡率为32%。这一过程的风险收益的令人堪忧,尤其是在老年患者中,此问题更加突出。 本研究的第一作者Jalbert JJ博士来自美国马萨诸塞州波士顿哈佛医学院,她说:“这些结果引发了颈动脉支架是否值得使用的争议。如果它的使用增加围术期风险或者患者并不能延长生命,那么有必要叫停CAS。”“
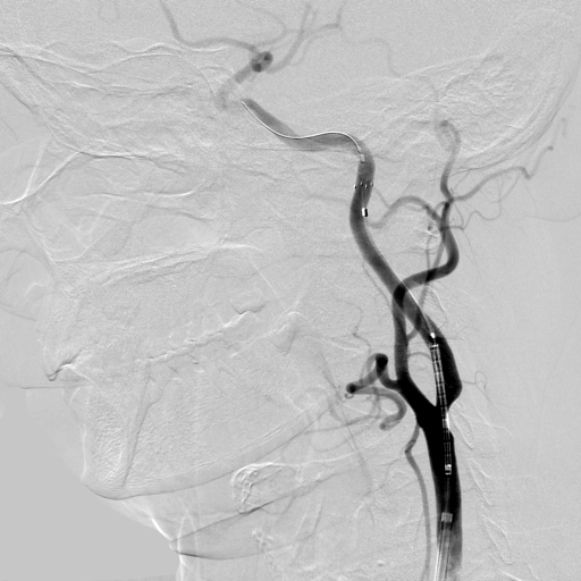
一项新的研究提出,患者接受颈动脉支架置入术(carotid artery stenting,CAS)2年后的死亡率为32%。这一过程的风险收益的令人堪忧,尤其是在老年患者中,此问题更加突出。
本研究的第一作者Jalbert JJ博士来自美国马萨诸塞州波士顿哈佛医学院,她说:“这些结果引发了颈动脉支架是否值得使用的争议。如果它的使用增加围术期风险或者患者并不能延长生命,那么有必要叫停CAS。”
“是否使用CAS应取决于患者总体生存率和并发症风险,以及对生活质量的影响。”他们总结道。“当决定医疗保险受益人是否接受颈动脉支架治疗时,对围术期高风险、年龄竞争负担以及合并症负担需慎重考虑。”
该分析于1月12日在线发表 JAMA Neurology。
研究者分析了22516名美国医疗保险受益人(平均年龄为76岁)的数据,他们在2005年至2009年间接受了CAS治疗。
在第30天,1.7%的患者死亡,33.3%的患者卒中或短暂性脑缺血发作(TIA),并且2.5%的患者出现心肌梗塞。围术期术中和术后,老年人群的颈总动脉狭窄和非选择性入院与死亡、卒中和TIA风险相关并增加。
在为期2年的随访中,平均死亡率占总纳入人群的32.0%。在出现症状的患者中高达37.3%;无症状患者的死亡率为27.7%(二者均在2年随访期间所获得的数据)。
作者指出,两项随机试验显示,颈总动脉支架术和颈总动脉内膜切除术具有类似的结果,但在实际临床中,患者有所区别。因为年龄越大的患者并存的疾病就越多,他们接受手术治疗的概率要更低一些。
在目前的研究中确实如此,患者的平均年龄是76岁,具有并存疾病高发率:患有缺血性心脏病人所占比例为85%,25%具有心脏衰竭,20%的人患有癌症。此外,大多数医师不符合设定CREST和SAPPHIRE试验的能力要求。
研究者总结道,“诸如SAPPHIRE或CREST对医保人群的概化试验存在局限性,注重强调还需评估真实世界中颈总动脉支架术的疗效。”
他们强调,需谨慎考虑围术期并发症高风险与年龄相关并存疾病风险负担。针对颈总动脉支架术、颈总动脉内膜切除术和药物保守治疗的选择,还需依靠真实世界中观察性研究来决定。
还需指出,预计颈总动脉支架术可降低5年卒中绝对风险,除缺血性中风引发死亡之外的诱因依然存在较高风险,这一获益可能会对其大打折扣。
这项研究由美国卫生和人类服务部拨款资助,贾尔伯特医生和艾伯茨博士宣告无相关财务关系。
原始出处:
Jalbert JJ, Nguyen LL, Gerhard-Herman MD, Jaff MR, White CJ, Rothman AT, Seeger JD, Kumamaru H, Williams LA, Chen CY, Liu J, Tsai TT, Aronow HD, Johnston JA, Brott TG, Setoguchi S.Outcomes After Carotid Artery Stenting in Medicare Beneficiaries, 2005 to 2009.JAMA Neurol. 2015 Jan 12. doi: 10.1001/jamaneurol.2014.3638.
Alberts MJ.Carotid Stenting-Why Treating an Artery May Not Treat the Patient.JAMA Neurol. 2015 Jan 12. doi: 10.1001/jamaneurol.2014.4142
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#颈动脉支架#
36
#Neurol#
30
#颈动脉#
32
#颈动脉支架置入术#
0
#置入术#
35
患者接受颈动脉支架置入术(carotid artery stenting,CAS)2年后的死亡率为32%。这一过程的风险收益的令人堪忧,尤其是在老年患者中,此问题更加突出。真要思考其必要性了
83