Clin Trans Gastroenterology:预防性抗结核治疗与接受抗TNF治疗的克罗恩病患者疾病进展加速有关
2022-07-06 xuyihan MedSci原创
克罗恩病(crohn disease,CD),又称局限性回肠炎、局限性肠炎、节段性肠炎和肉芽肿性肠炎、也译为克隆氏病,是一种原因不明的肠道炎症性疾病。
克罗恩病 (CD) 是一种复杂且易复发的胃肠道疾病,能逐渐发展为狭窄或穿透性病变。抗肿瘤坏死因子-α(抗-TNFα)药物等生物制剂彻底改变了CD的治疗方法,并在实现临床缓解和黏膜愈合方面具有公认的功效。然而,机会性感染的风险,例如激活潜伏性结核感染 (LTBI),仍然是一个棘手的问题。为防止LTBI激活,指南建议在开始抗TNF治疗之前进行结核病暴露史、干扰素-γ释放试验、结核菌素皮肤试验和胸部影像学检查。另外指南建议对患有LTBI的CD患者进行预防性抗结核治疗 (ATT),例如异烟肼 (INH) 和利福平 (RFP) 单药治疗或联合治疗,这已被证明是降低接受抗结核药物治疗的CD患者TB活化的有效策略。
然而,预防性 ATT 可能会导致潜在的副作用。最近的一项研究引起了对在CD诊断前有经验性ATT治疗的 CD 患者的担忧,因为他们更容易出现肠道狭窄。因此,本项研究的目的是比较 ATT 使用者和非 ATT 使用者在接受抗 TNF 治疗的 CD 患者中疾病进展的差异。
为此,研究人员在出现炎症行为 (B1) 并接受抗 TNF 药物治疗的 CD 患者中进行了一项回顾性、多中心研究。疾病进展被定义为出现狭窄(B2)或穿透(B3)的表型。ATT使用者与非 ATT使用者进行了的倾向得分相匹配。生存和多变量 Cox 分析用于确定与疾病进展相关的因素。
本项研究共招募了441名患者,包括295名ATT用户和146名非ATT用户,中位随访时间为3.15年。在1年、3年、5年和10年的随访后,ATT组的累积疾病进展率持续高于非 ATT组(P=0.031)。多变量Cox分析使用整体(风险比=2.22;95%置信区间:1.11-4.48; P=0.025)和倾向得分匹配队列(风险比=2.35;95%)将ATT确定为疾病进展的独立危险因素(置信区间:1.07–5.14;P= 0.033)。在亚组分析中,与接受ATT<4.5个月(P=0.005)和非ATT治疗(P=0.036)的患者相比,接受 ATT≥4.5个月的患者疾病进展率显着更高。
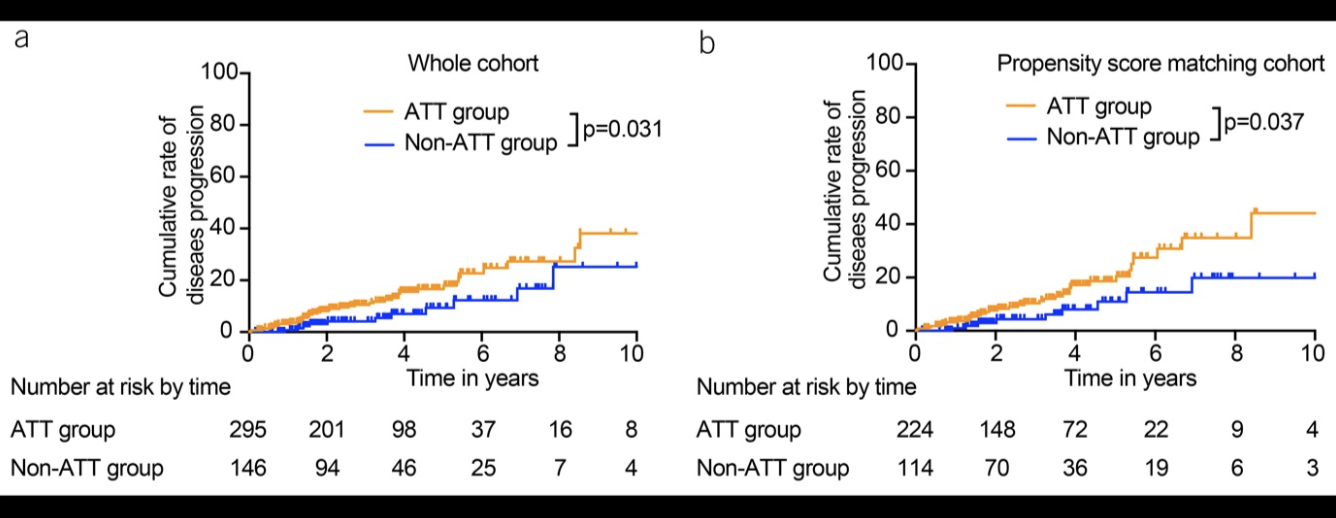
本项研究结果证实持续时间超过4.5个月的预防性ATT治疗与接受抗TNF治疗的CD患者的疾病进展相关。
原始出处:
Liu, Fen. Et al. Prophylactic Antitubercular Therapy Is Associated With Accelerated Disease Progression in Patients With Crohn's Disease Receiving Anti-TNF Therapy: A Retrospective Multicenter Study. Clinical and Translational Gastroenterology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#抗TNF治疗#
46
#Gastroenterol#
46
#AST#
43
#预防性#
40
#抗TNF#
43
#GAS#
33
#疾病进展#
39
#TRA#
26
学习了!
48
好文章,谢谢分享。
37