Allergy:高山气候疗法可促进不同哮喘表型患者的免疫调节作用
2022-02-11 小文子 MedSci原创
鉴于未控制哮喘患者的炎症和免疫调节作用降低,AACT被认为是自然的靶向生物疗法。
欧洲高海拔气候疗法(AACT)结合了高海拔的物理特征和避免高山气候中的环境触发因素,以及多学科肺康复方法。AACT可改善哮喘患者的临床表现和呼吸功能参数,然而使患者获益的海拔高度特征和高山气候影响的机制尚不清楚,Allergy杂志的一项研究描述了中等海拔地区高山气候的环境特征、免疫调节作用、多学科肺康复方法及其对未控制和重度哮喘的临床影响。

两名专家回顾了以下主题的相关文献:海拔高度特征、高山气候环境特征、免疫学结局、成人临床结局、儿童临床结局。使用Medline、Embase和Cochrane数据库进行检索,纳入2021年4月24日前发表的论文。根据海拔高度对健康人体生理和健康的影响,将海拔高度分为低(<1200m〉、中(1200m-2500m)、高(2500m-3500m)、极高(35005800m)和极高(>5800m)海拔。大多数欧洲高原诊所位于海拔1200米到2500米之间的阿尔卑斯山脉,该地缺氧不会对身体造成过度的压力。
中海拔地区的气压、氧分压和空气密度降低,温度和湿度相对较低,紫外线辐射增加,诱发了多种生理和免疫适应反应。缺氧生理反应的主要调节因子是在广泛的免疫和组织固有细胞中表达的缺氧诱导因子1a (HIF-1a)。高海拔地区的研究表明,不同程度的缺氧相关免疫调节可能在中海拔地区已经开始。
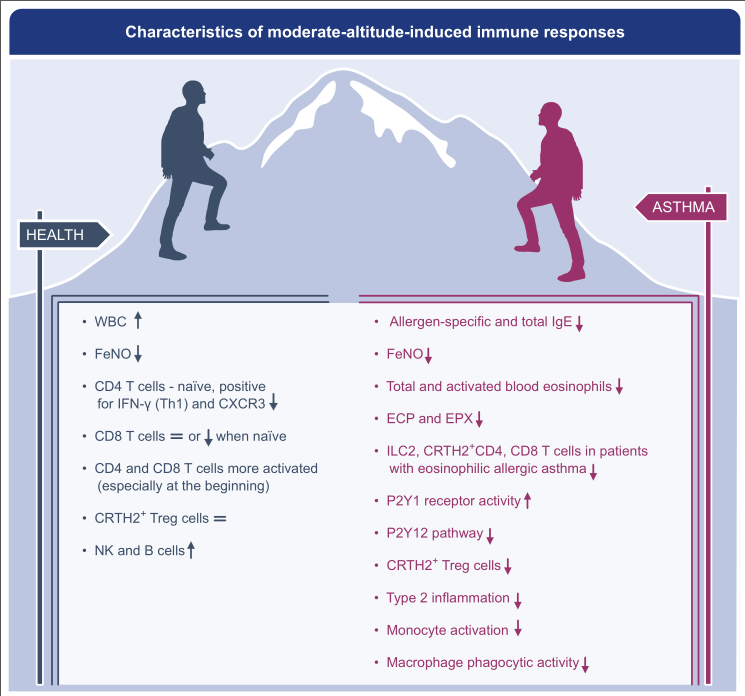
高山气候的环境特征包括减少空气过敏原,如室内尘螨(HDM)、花粉、真菌,并减少空气污染和不同微生物暴露。这些综合因素似乎具有免疫调节作用,控制致病性炎症反应,并有利于减少不同哮喘表型患者的神经免疫应激。海拔对不同哮喘表型的免疫结果可能有不同的影响,使过敏性哮喘患者的2型炎症减轻。高海拔恢复了哮喘表型中Tregs的抑制和调节表型。
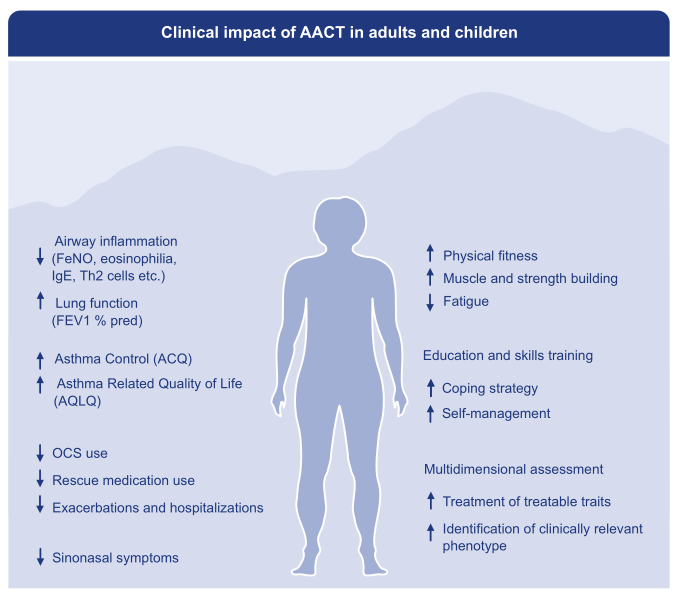
AACT项目包括患者评估、心理和行为干预、个性化锻炼项目、患者教育和治疗结束后的个性化行动计划。主要作用可能是由于炎症快速减轻,或高山气候环境触发因素较少,或海拔气候因素及其免疫调节作用。
AACT的多学科治疗方案可进一步改善患者的哮喘控制和生活质量,如减少哮喘急性加重和住院,减少口服糖皮质激素(OCS)的需要,改善肺功能,降低气道高反应性(AHR),提高运动耐力,改善鼻腔预后。
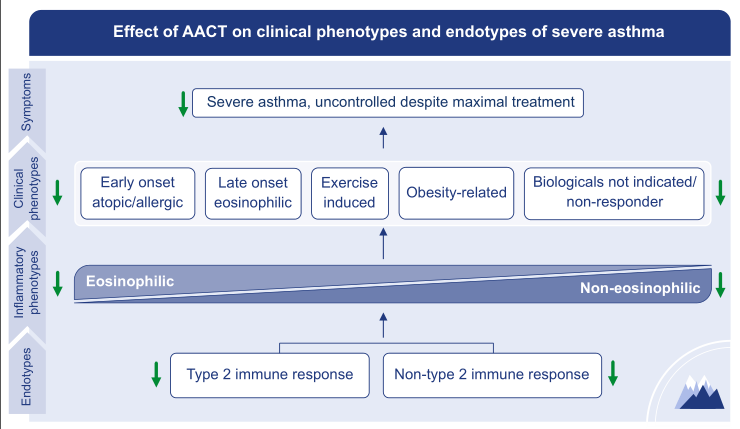
基于观察性研究和专家意见,AACT是所有哮喘表型患者的一种有价值疗法,根据指南在医学科学和治疗方面取得的进展,这些患者无法实现复杂疾病的最佳控制,因此,患者存在身心健康受损的风险。鉴于未控制哮喘患者的炎症和免疫调节作用降低,AACT被认为是自然的靶向生物疗法。
原文出处:
K.B. Fieten M.T. Drijver-Messelink, et al, Alpine Altitude Climate Treatment for severe and uncontrolled asthma: an EAACI Position Paper,Allergy,2022, doi:10.1111/ALL.15242.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好文章
33
#ALL#
42
#表型#
34
新方法。有用
66
好文章,学习到了,谢谢。
59
好文章,学习到了,谢谢。
0