糜坚青教授:CAR-T治疗新近进展及安全性管理策略
2018-01-10 佚名 肿瘤资讯
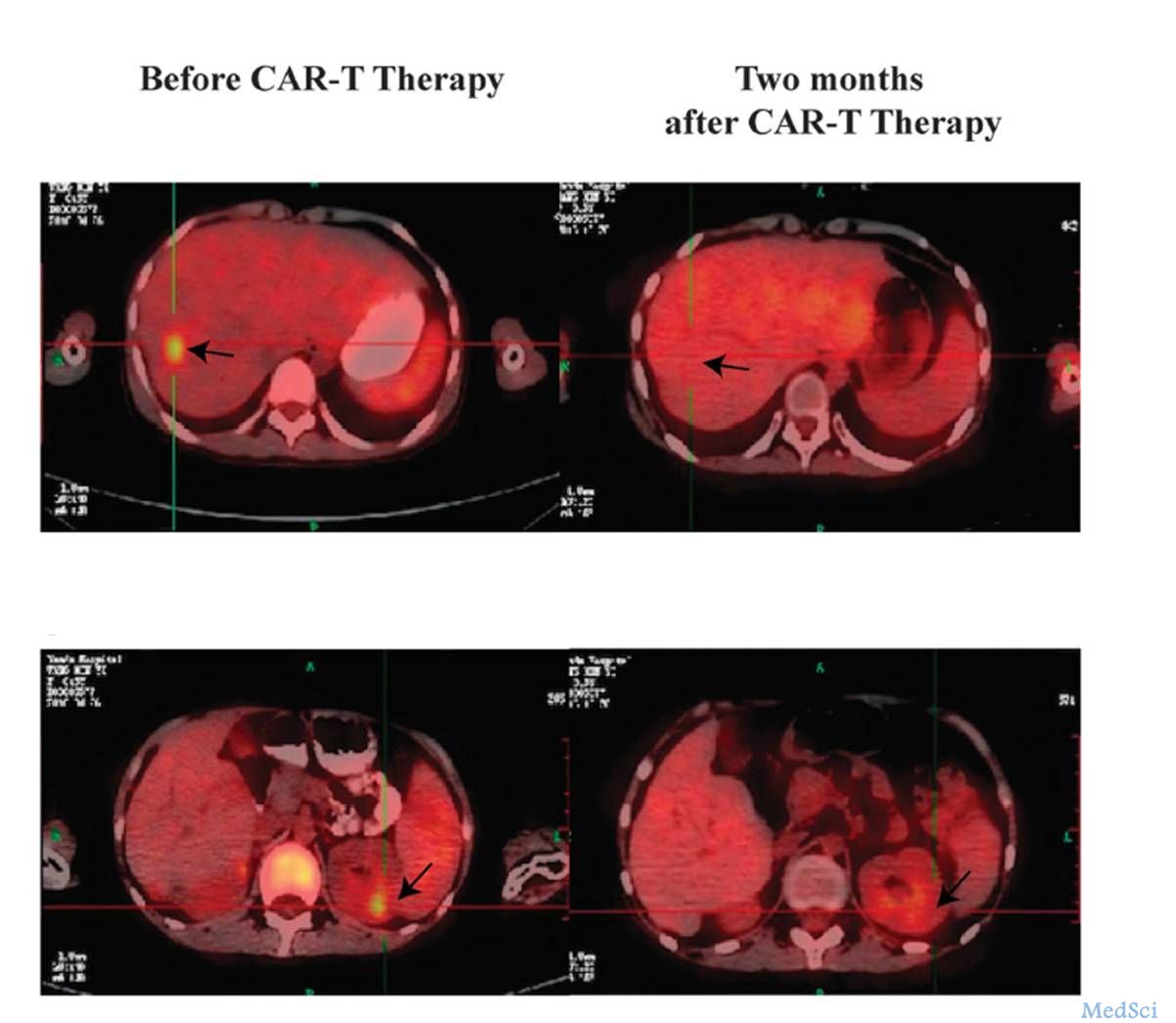
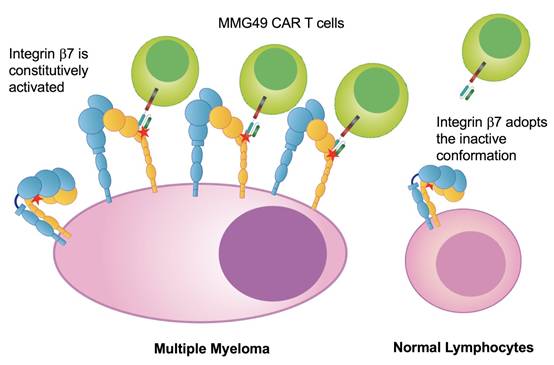
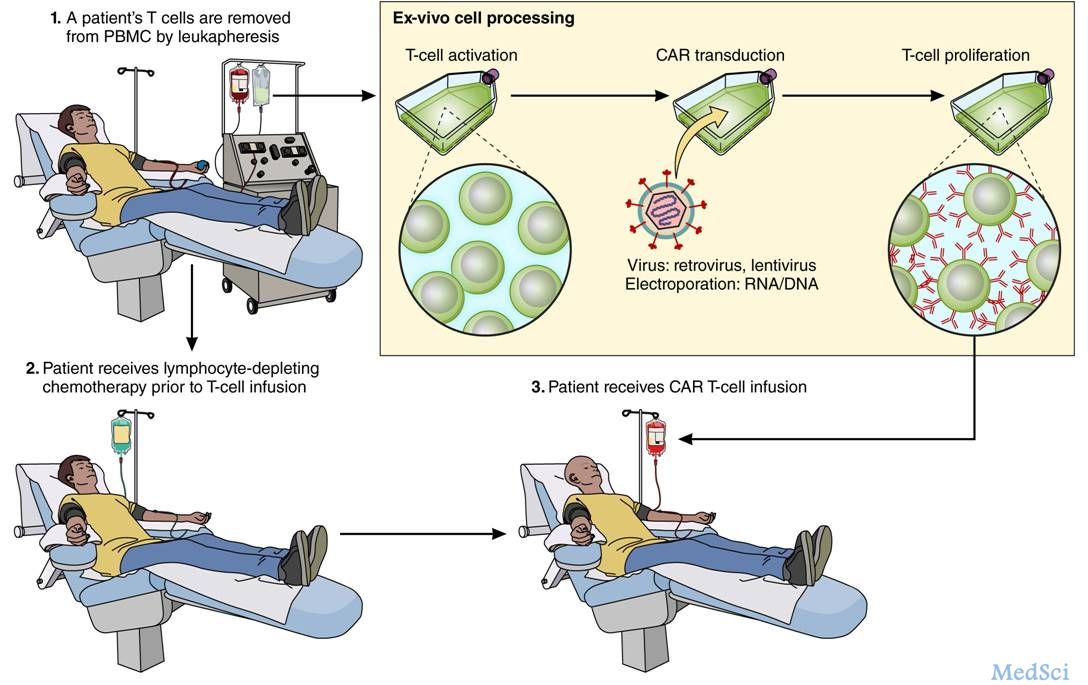
嵌合抗原受体T细胞免疫治疗(CAR-T)通过特异性识别肿瘤相关抗原,进而使经过修饰的效应T细胞对肿瘤细胞具有更强、更持久的靶向杀伤性。目前,CAR-T在复发/难治B细胞恶性肿瘤的治疗中具有良好的疗效,并成为近年来炙手可热的恶性肿瘤研究方向之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#管理策略#
27
#CAR-#
35
#安全性管理#
44
henhao
62
学习了新知识
61