JGH:肝细胞癌——手术切除与TACE孰优?
2014-01-14 MedSci MedSci原创
韩国成钧馆大学医学院的Moon Seok Choi医生和他的同事们对手术切除肝巨大肿瘤和肝动脉化疗栓塞的远期疗效进行了对比,并对与生存期有关的预后因素进行了评估。自2000年至2009年,有84位患者进行了手术切除,267位患者行肝动脉化疗栓塞。研究者们收集了患者的年龄、性别、肝病病因、是否存在肝硬化和肝功能分级,以及肿瘤大小、数目、范围和血管侵蚀情况的数据信息。主要评价项目是总生存期。其他评
韩国成钧馆大学医学院的Moon Seok Choi医生和他的同事们对手术切除肝巨大肿瘤和肝动脉化疗栓塞的远期疗效进行了对比,并对与生存期有关的预后因素进行了评估。
自2000年至2009年,有84位患者进行了手术切除,267位患者行肝动脉化疗栓塞。研究者们收集了患者的年龄、性别、肝病病因、是否存在肝硬化和肝功能分级,以及肿瘤大小、数目、范围和血管侵蚀情况的数据信息。 主要评价项目是总生存期。其他评价项目还包括总生存期的预后因素。该评价项目主要是通过分数匹配的队列的单变量和多变量分析得出的。该队列有76个年龄、性别、肝病病因、肝功能分级、肿瘤数量、血管侵蚀情况、肿瘤范围与试验组匹配的患者组成。 进行外科手术的患者在前两年内每3个月复查一次,之后每6个月复查一次。复查时进行肝功能测试、血清甲胎蛋白水平测试和肝动态CT来监测肿瘤有无复发。 那些进行肝动脉化疗栓塞的患者在第一个月时进行两次连续的监测,然后每个治疗周期之后的1个月在门诊复查。复查时他们进行类似电池的试验来判断肿瘤分期。如果肝动态CT发现肿瘤后,需要再次进行肝动脉化疗栓塞。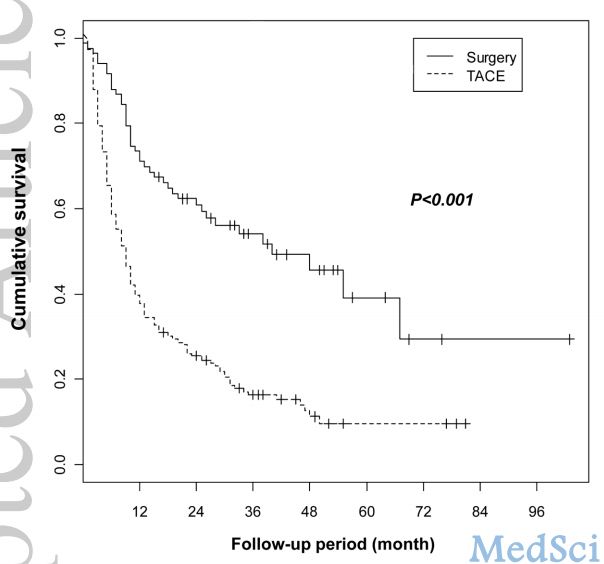
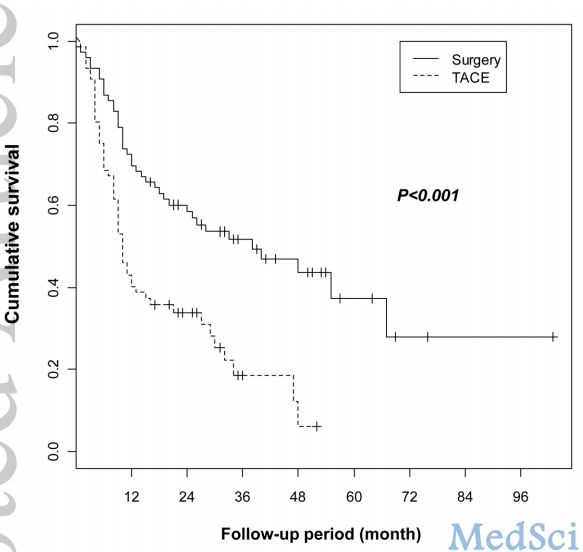
Figure
2. Kaplan-Meier survival curves showing overall survival rates in
propensity score matched-cohort (76 matched pairs) with huge
hepatocellular carcinoma after surgery and TACE. Surgery group showed
higher 1-, 2-, and 3-year survival rates than TACE group (69.7%, 58.6%,
and 51.7% vs. 40.2%, 33.9%, and 18.5%, respectively; P<0.001).
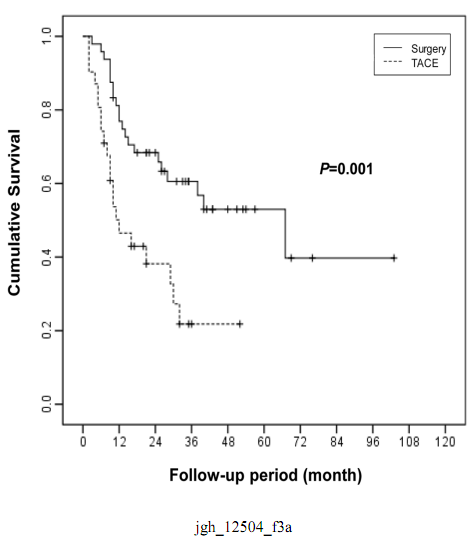
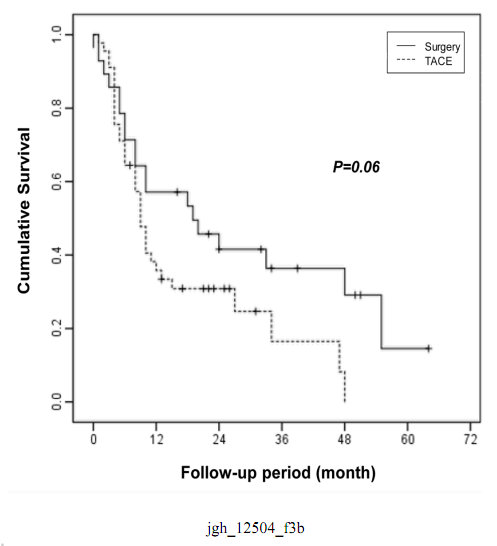
Figure
3. Kaplan-Meier survival curves showing overall survival rates
cirrhosis after surgery and TACE in propensity score matched-cohort (76
matched pairs) according to the presence of cirrhosis: a) in
non-cirrhotic patients and b) in cirrhotic patients.
作者们警示,尽管外科手术后1年、3年、5年患者的生存率较高,但是非手术治疗组患者肝硬化、门静脉或肝静脉侵蚀的发生率较低。患者选择治疗方式的不同可能对结果有一定影响,这使这一研究的价值受到一定的限制。 他们也注意到,这一研究是一个回顾性研究,患者的数量较少,且研究只关注了血管侵蚀的情况,而没有对比血管侵蚀的范围,这些都限制了这一研究的价值。 MedSci评论:这个研究最大特色在于采用了倾向匹配得分方法,纠正了两种的基线差异。否则如果不纠正这种差异,会带来大量的偏倚。因为能手术的患者,肿瘤侵袭范围,肿瘤结节的数量,以及肿瘤的位置可能都较好。而TACE的患者可能状况更差,因此,很难进行比较。采用倾向匹配得分,修正这些差异,结论会更令人信服。 原始出处: Yang Won Min, et al. Long-term survival after surgical resection for huge HCC: comparison with TACE after propensity score matching.Journal of Gastroenterology and Hepatology 10.1111/jgh.12504
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TAC#
33
#肝细胞#
34
#细胞癌#
34
#ACE#
42
#手术切除#
0
MedSci评论值得看
125