Chin J Cancer Res:中肿徐瑞华教授团队IV期观察性研究:评估中国转移性结直肠癌使用化疗联合贝伐珠单抗治疗的真实世界疗效和安全性
2021-12-22 yd2015 MedSci原创
这项观察性IV期试验扩大了我们对贝伐珠单抗在中国人群中的应用经验,并为其整体疗效和安全性提供了良好的指示。贝伐单抗联合化疗改善中国mCRC患者预后,并且安全可控。
贝伐珠单抗在改善全球转移性结直肠癌(mCRC)患者的预后方面具有重要和不断发展的作用,并于2010年在中国获得批准。然而,关于化疗方案联合贝伐珠单抗在中国mCRC患者中的疗效和安全性的真实世界数据有限。来自中山大小肿瘤防治中心徐瑞华教授团队联合国内多家医院开展了观察性IV期临床研究,评估贝伐珠单抗联合化疗在中国mCRC患者中的疗效和安全性。相关结果发表在Chinese Journal of Cancer Research杂志上。

2013年9月至2016年11月,该前瞻性、多中心、观察性、非干预性IV期临床研究纳入中国26个中心的经组织学证实的mCRC患者。符合条件的患者接受不同化疗方案联合贝伐珠单抗治疗。分析意向治疗研究人群的疗效和安全性数据。
共纳入613例患者进行安全性分析,611例进行疗效分析。中位年龄55岁(范围16-85岁),男性384例(62.64%)。在447名接受评估的患者中,有426例(95.30%)患者ECOG PS为0-1。169例接受检测的患者中有98名(57.99%)患者发现KRAS突变。
患者接受贝伐单抗的中位剂量为33.23 mg/kg (范围2.73 3288.00),中位周期为9周期(范围1-53)。343例(55.95%)患者接受一线贝伐单抗治疗,270例(44.05%)患者接受二线贝伐单抗治疗。化疗方案以伊立替康为基础方案(62.32%)、奥沙利铂为基础方案(60.85%)、卡培他滨为基础方案(28.38%)。

常用的化疗方案
随访中位时间9.21个月(范围0.03-33.87个月),611例患者中有280例(45.83%)在随访结束时死亡。总体人群中位OS为18.00个月(95% CI, 16.99-20.07),中位无进展生存期(PFS)为10.05个月(95% CI, 9.20-11.37)。ORR为21.00%,DCR为89.40%。
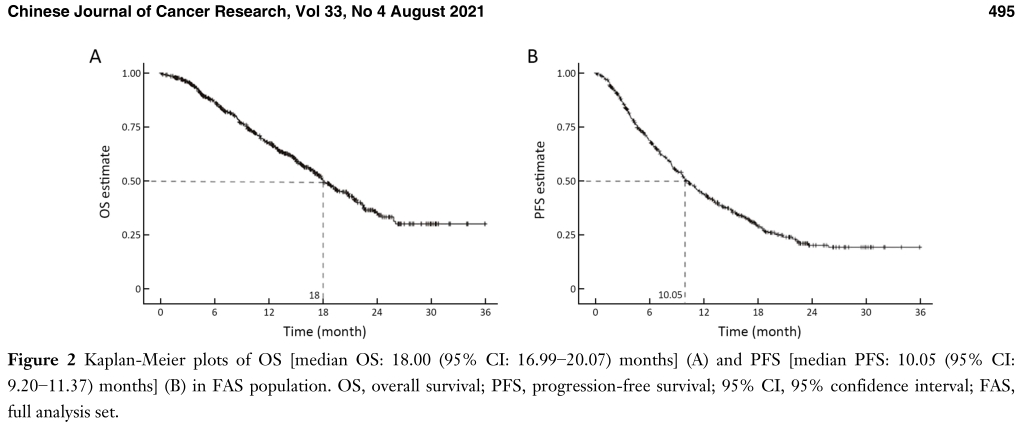
OS和PFS
接受一线治疗的患者的中位OS跟接受二线治疗的类似,分别为 18.00个月 (17.08−21.82) 和17.45个月(14.72−20.07)。而接受一线治疗的患者的中位PFS长于接受二线治疗的患者(11.04个月vs. 8.74个月)。接受一线治疗的患者也有更高的ORR(27.08% vs 13.45%)。一线治疗和二线治疗的DCR分别为92.78%和85.20%。

疗效评估
在亚组分析中,未观察到年龄、KRAS突变状态、原发肿瘤部位、原发肿瘤切除和不同化疗方案之间的显著差异。然而,根据转移状态、治疗时间和血压升高观察生存差异。异时转移患者的中位PFS比同时转移患者短(9.20个月vs. 10.97个月;P = 0.044)。治疗时间越长,生存率越高。以8周为截止时间,接受>8周治疗的患者与接受≤8周治疗的患者相比,中位OS有显著改善(19.15个月vs 17.81个月;p<0.001)。血压升高患者的中位OS比无血压升高的患者长(20.80个月vs. 16.66个月;P = 0.002)。

亚组分析
所有患者(n=613)均可进行安全性评估,共有569例(92.82%)患者报告了至少1种AE,有151例(24.63%)患者发生了3级及以上的AE。最常见的AEs为白细胞减少症(39.97%)、恶心(39.31%)、中性粒细胞减少症(29.04%)、呕吐(27.24%)、食欲不振(23.16%)、高血压(19.25%)、腹泻(18.76%)和贫血(17.78%)。SAEs的发生率为27例(4.40%),包括中性粒细胞减少、死亡、白细胞减少、腹泻、肺部感染和造口相关出血。贝伐单抗相关AEs有288例(46.98%)。特别关注AE有31例(5.06%),包括高血压(12例)、脓肿瘘管(7例)、出血(6例)、蛋白尿(3例)、胃肠道穿孔(2例)、静脉血栓事件(1例)。31例(5.06%)患者因AEs停药。76例患者(12.40%)进行了剂量调整。
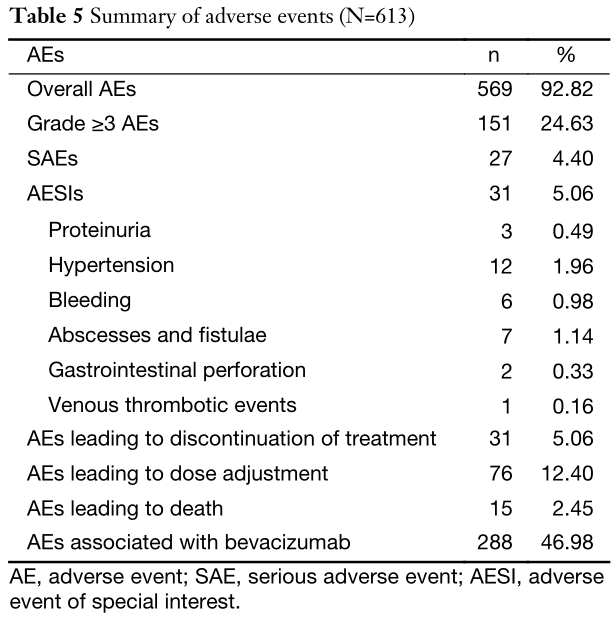
AEs
综上,这项观察性IV期试验扩大了我们对贝伐珠单抗在中国人群中的应用经验,并为其整体疗效和安全性提供了良好的指示。贝伐单抗联合化疗改善中国mCRC患者预后,并且安全可控。
原始出处:
Wang F, Dai G, Deng Y, Tang Y, Wang W, Niu Z, Bi F, Zhu L, Guo Z, Yan J, Hu B, Tao M, Yang S, Zhang S, Wen L, Xu R. Efficacy and safety of chemotherapy combined with bevacizumab in Chinese patients with metastatic colorectal cancer: A prospective, multicenter, observational, non-interventional phase IV trial. Chin J Cancer Res. 2021;33(4):490-499. doi: 10.21147/j.issn.1000-9604.2021.04.06.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#贝伐珠#
41
#疗效和安全性#
45
#真实世界#
44
#转移性#
49
#结直肠#
0
#贝伐#
28
#观察性研究#
38
太棒了
62