CELL METAB:高脂食品如何引发心血管疾病?激活炎症反应!
2017-02-15 佚名 生物探索
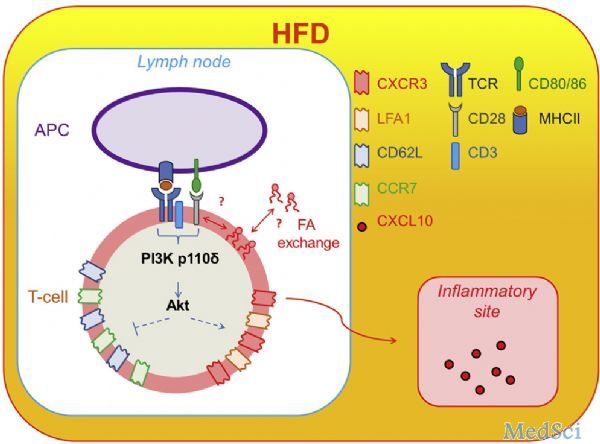
众所周知,肥胖和高脂饮食是导致心血管疾病的罪魁祸首之一。来自玛丽皇后学院的一项研究认为,机体的免疫应答在这一过程中起着关键作用。高脂食品或肥胖可以导致更多T细胞发育成为效应记忆CD4 + T细胞,从而使炎性反应被过度激活,最终引发心血管疾病。这一研究发表于Cell Metabolism杂志上。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#MET#
34
#CEL#
23
#Cell#
30
#Meta#
32
#炎症反应#
28
#血管疾病#
18
#高脂#
29
看来老外的身体素质不必我们想象中的好?
59