Heart:左室功能障碍的超声心动图特征与慢性肾脏病患者预后
2022-09-05 MedSci原创 MedSci原创
HF与随后较差的临床结局相关,这在HFrEF患者中可能更明显,其次是HFmrEF和HFpEF患者,相对于非HF组。
慢性肾脏病被认为是世界范围内的健康负担,每年造成约85万人死亡,影响美国约17%的成年人群。慢性肾脏病患者常见左室(LV)结构和功能异常,30%-60%的慢性肾脏病患者会出现射血分数保留或减少的心力衰竭(HF)。慢性肾脏病和HF之间的关系往往因双向因果关系而且相对复杂。HF给慢性肾脏病患者带来了巨大的负担,并且HF的患病率很高。HF会导致患者多次住院,但HF亚型是否加重慢性肾脏病患者的长期预后和肾功能仍不确定。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究对象为2011年1月1日至2018年12月31日期间接受超声心动图检查的10904例年龄≥20岁的慢性肾脏病患者。

研究人员将患者分为四组:非HF组、射血分数降低的HF组(HFrEF)、射血分数轻度降低的HF组(HFmrEF)和射血分数保留的HF组(HFpEF)。该研究的主要终点为全因死亡率、主要不良心血管事件(MACE)和不良肾脏结局。
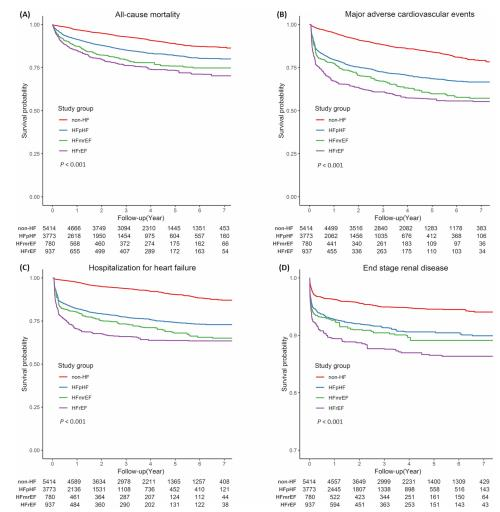
研究人员采用治疗加权校正的反概率法分析发现HFrEF组的全因死亡和MACE相对于非HF组的风险最大(风险比为3.18(95%CI为2.57~3.93)和风险比为3.83(95%CI为3.20~4.59)),其次是HFmrEF(风险比为2.75(95%CI为2.22~3.42)和风险比为3.08(95%CI为2.57~3.69))和HFpEF(风险比为1.85(95%CI为1.59~2.15)和风险比为2.43(95%CI为2.16~2.73)组。此外,与其他组相比,HFrEF组发生终末期肾脏疾病的风险最大(风险比为2.58(95%CI为1.94-3.44))。
由此可见,HF与随后较差的临床结局相关,这在HFrEF患者中可能更明显,其次是HFmrEF和HFpEF患者,相对于非HF组。
原始出处:
Shuo-Ming Ou.et al.Echocardiographic features of left ventricular dysfunction and outcomes in chronic kidney disease.heart.2022.https://heart.bmj.com/content/early/2022/08/28/heartjnl-2022-321404
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#患者预后#
113
#心动图#
120
#左室功能#
101
#ART#
116
#功能障碍#
187
#HEART#
151
#慢性肾脏#
120