CASE M25 年轻男性,已知有类固醇治疗狼疮性肾炎史。伴有双侧髋关节疼痛和运动困难的抱怨。



不规则的透光区,代表软骨下囊变,与边缘硬化在两个股骨头。双股骨头呈线性软骨下骨折/断裂,伴有轻度塌陷/扁平。这些发现代表了双侧股骨头缺血性坏死。
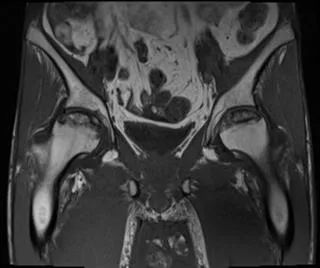
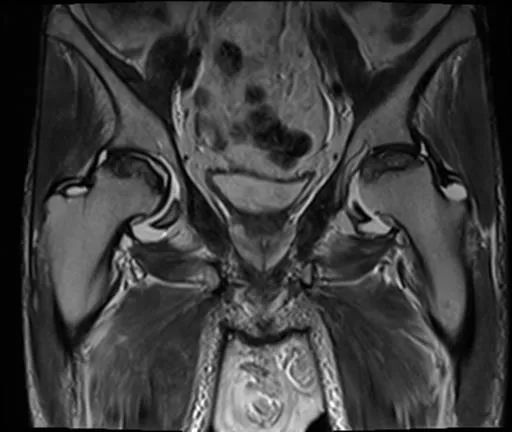
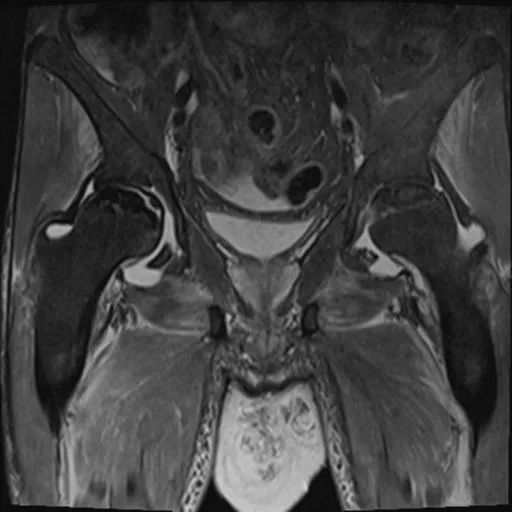
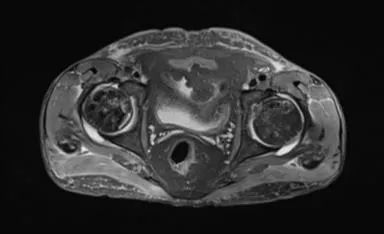
双侧股骨头前上面有大面积的骨髓异常,T1为低信号,在T1和T2W图像上,周围环绕着低强度的边缘。双股骨头呈线性软骨下骨折/断裂,在脂肪抑制图像上得到很好的评价。两侧均有轻度塌陷/扁平的轻微轮廓畸形。这些发现代表了双侧股骨头缺血性坏死。
骶髂关节和耻骨联合正常。
盆腔内存在小体积游离液。弥漫性软组织水肿见于前腹壁及骨盆、大腿。这些发现是由于慢性肾脏疾病造成的。
这是典型的双边缺血性坏死有特征性的X线和MRI表现。患者有SLE合并狼疮性肾炎并接受类固醇治疗,均易发生AVN。
文章精选
正常关节软骨的MRI表现,基本功掌握!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#骨头#
36
#缺血性#
36
#坏死#
31
#股骨#
44
#股骨头#
43