原创靶标,抑制结肠癌转移的“新武器”——专访上海交大医学院张健教授
2018-02-28 佚名 学术经纬
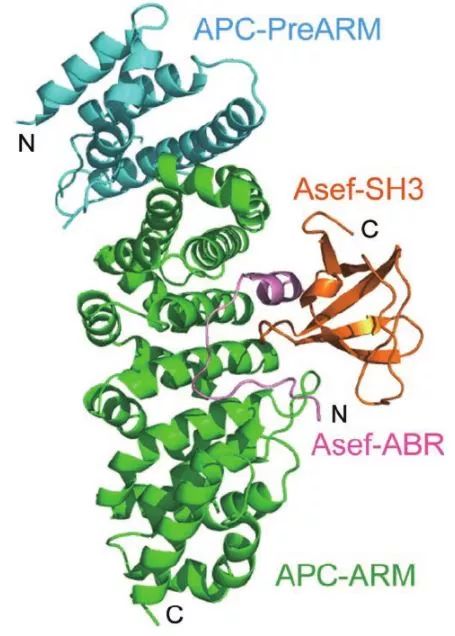
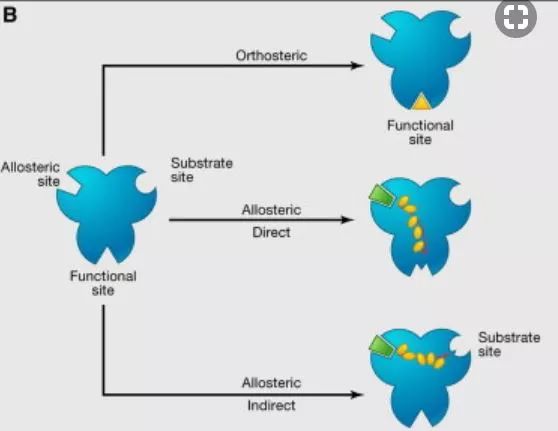
<!--ewebeditor:page title=""--> <div>据国家癌症中心最新发布的《2017中国肿瘤现状和趋势》,结、直肠癌发病率在中国男性患者中位居第五,在女性患者中则进入前三名。以总体肠癌发病人数而言,中国患者人数已跃居世界第一位。90%的恶性结肠肿瘤均由结肠息肉发展而来,其中腺瘤性息肉的恶变几率远远超过普通炎性息肉。<a class="channel_keylink" href="http://edu.medsci.cn/course/search.do?w=%E4%B8%B4%E5%BA%8A" target="_blank">临床</a>研究表明<a class="channel_keylink" href="http://www.medsci.cn/article/list.do?q=%E7%BB%93%E8%82%A0%E7%99%8C">结肠癌</a>发病常常表现出家族性,且60%患者体内存在腺瘤性息肉易感蛋白(Adenomatous Polyposis Coli,APC )编码基因突变,该突变在癌细胞转移过程中扮演了重要角色。</div><d

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#医学院#
29
#专访#
30
学习了谢谢分享!!
47
#上海交大#
34
#靶标#
26
#癌转移#
21
学习了.谢谢分享
61
阅
53
阅
50
好消息啊
51