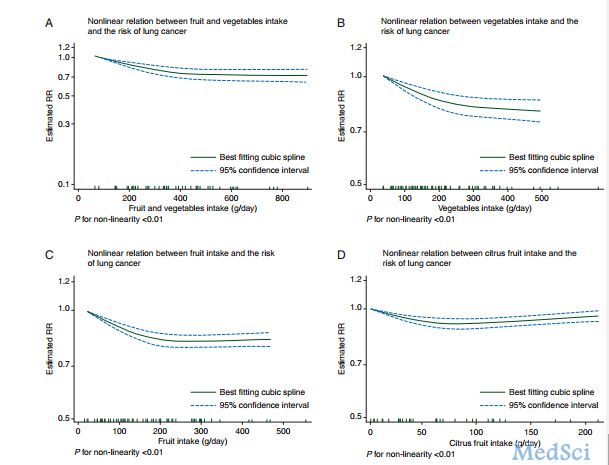
NEJM:中国人多吃水果可降低心血管疾病风险(Kadoorie Biobank研究)
2016-04-07 崔倩 译 MedSci原创
在西方人群中,较高水平的水果消费与心血管疾病风险较低有关,但在中国却很少有人了解上述联系,中国消是一个费水平低且卒中发生率很高的国家。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
27
文章真心很好,感谢作者
50
不错不错
85
文章不错
103
值得关注
100
#疾病风险#
23
#血管疾病#
20
好喜欢
66
健康生活方式
78
Kadoorie数据库发表了大量高水平文章了
57