JAMA Ophthalmol:COVID-19诊断后视网膜血管闭塞发生率的变化
2022-04-24 从医路漫漫 MedSci原创
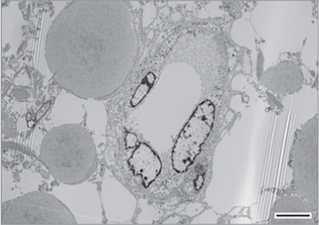
光学相干断层血管造影术研究发现,与对照组相比,COVID-19感染患者的视网膜血管密度减少。
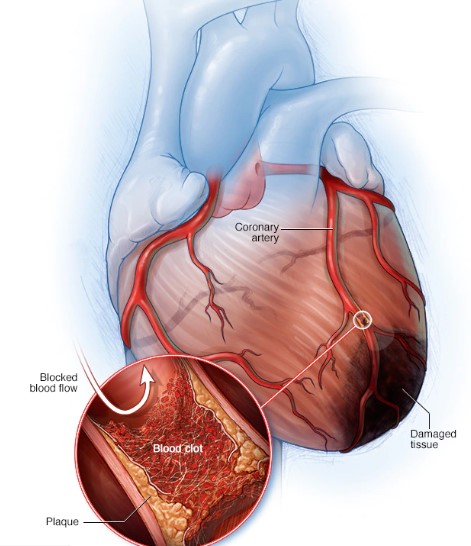
背景:新冠肺炎感染后可出现多器官病理,包括累及静脉和动脉系统的血管损伤。光学相干断层血管造影术研究发现,与对照组相比,COVID-19感染患者的视网膜血管密度减少。考虑到新冠肺炎感染引起的血栓前状态和观察到的视网膜血管变化,似乎很直观地将这种感染与视网膜血管阻塞联系起来;然而,关于可能联系的数据有限。
目的:探讨新冠肺炎感染后视网膜血管阻塞发生率的变化。
设计、设置和参与者:这项在一个综合性医疗保健组织(南加州凯撒永久医疗机构)进行的队列研究包括在2020年1月20日至2021年5月31日期间被诊断为新冠肺炎感染的无视网膜血管阻塞病史的患者。如果患者在被诊断为新冠肺炎之前有视网膜动脉阻塞(RAOS)或视网膜静脉阻塞(RVO)病史超过6个月,或者如果他们在新冠肺炎诊断之前在南加州凯撒永久医院注册不到6个月,他们就被排除在外。
暴露:新冠肺炎感染。
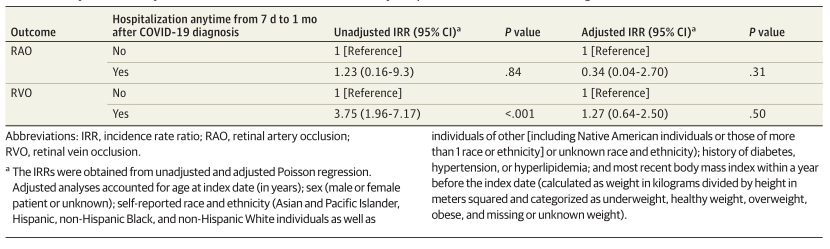
主要结果和措施:新冠肺炎诊断后新的RAO和RVO平均双周发病率的变化。在考虑了基线人口学特征、病史和住院情况后,计算调整后的发生率比(IRR)以比较新冠肺炎诊断前后视网膜血管阻塞的发生率。
结果:本研究共纳入432515例新冠肺炎感染者。平均年龄40.9岁(19.2岁),女性231767例(53.6%)。在新冠肺炎诊断后的6个月内,16例患者有RAO(粗发病率,3.00/100万患者),65例患者有RVO(粗发病率,12.20/100万患者)。在调整了年龄、性别、自我报告的种族和民族、体重指数、糖尿病、高血压或高脂血症病史和住院等因素后,新冠肺炎感染后6个月的新RVO发生率高于感染前6个月(调整后的IRR1.54;95%CI,1.05-2.26;P=.03)。新冠肺炎诊断后RAOS的发生率增加较小(IRR1.35;95%CI为0.64~2.85;P=0.44)。RAOS和RVOS的发病高峰分别出现在新冠肺炎确诊后10~12周和6~8周。
表1 相对于新冠肺炎诊断日期的RAO和RVO的平均发生率
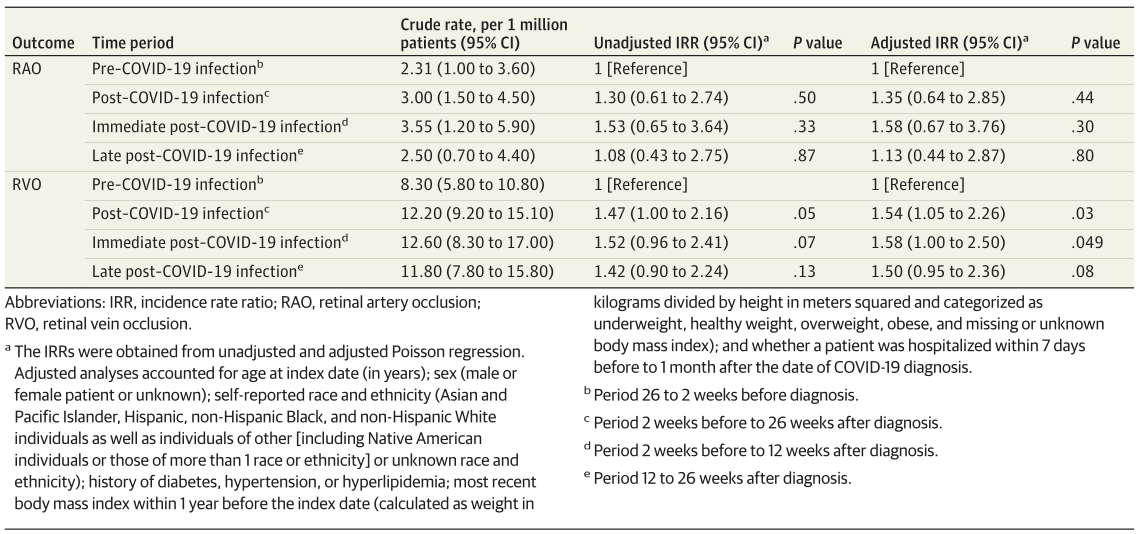
表2 根据视网膜血管阻塞状况分层的新冠肺炎感染患者的基线特征
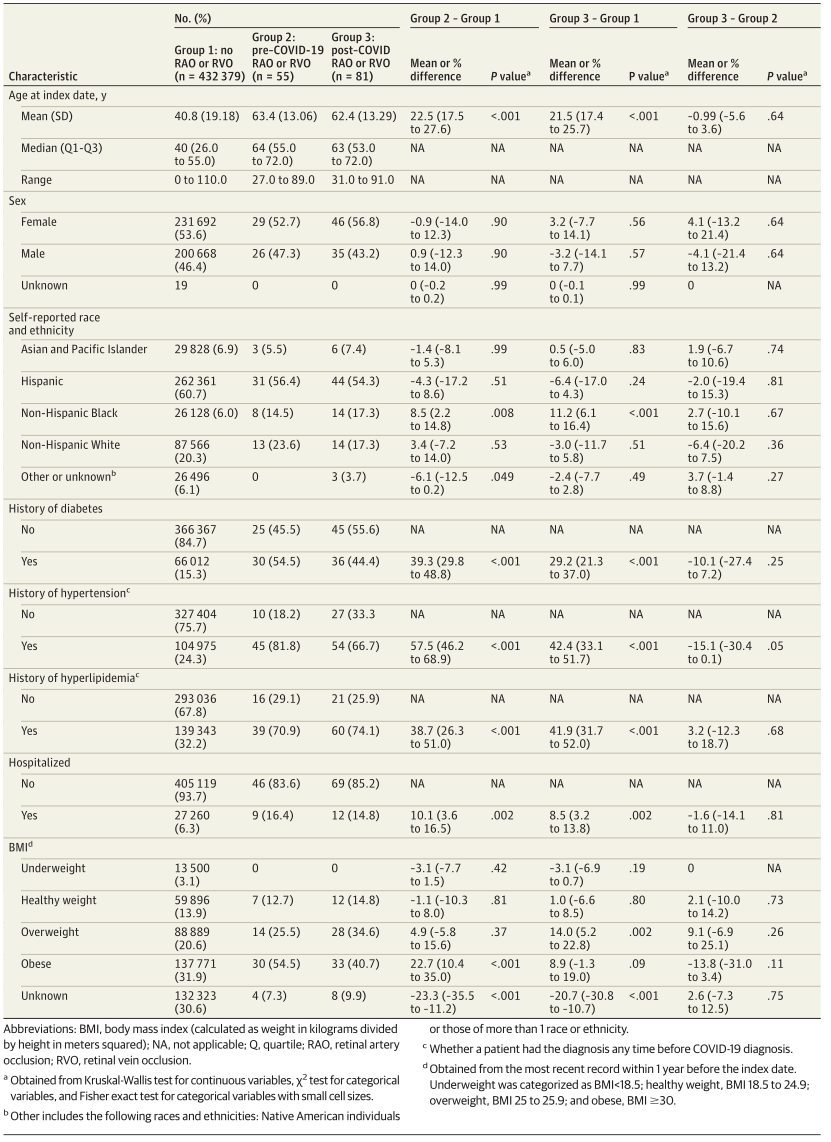
表3 新冠肺炎诊断后住院的视网膜血管阻塞的未校正和校正IRRs
结论:这项研究的结果表明,新冠肺炎感染后RVO的发生率有所增加;然而,这些事件仍然很少见,在没有随机对照的情况下,无法建立因果关系。有必要进行更大规模的流行病学研究,以更好地确定视网膜血栓栓塞症事件和新冠肺炎感染之间的联系。
原文出处:Modjtahedi BS, Do D, Luong TQ, Shaw J,Changes in the Incidence of Retinal Vascular Occlusions After COVID-19 Diagnosis.AMA Ophthalmol 2022 Apr 14
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管闭塞#
35
#发生率#
49
#视网膜#
36
#THA#
29
JAMA上文章都是顶级的,谢谢梅斯及时上新
32