European Radiology:可预测肾细胞癌切除术后复发风险的CT放射组学因素
2024-01-06 shaosai MedSci原创 发表于上海
放射组学是一个不断发展的领域,可对从医学成像中提取的定量特征进行计算机化分析。在肿瘤学中,放射组学旨在发现图像中可能与癌症生物学有关的隐藏模式并提供预后信息。
现阶段,手术切除仍然是肾细胞癌(RCC)治疗的主要手段。然而,非转移性疾病的肾切除术后有20%的复发率,增加了患者对辅助治疗方案的依赖。一些随机试验发现,辅助性的酪氨酸激酶抑制剂(TKIs)对非转移性RCC患者的生存率没有优势。然而,将所有非转移性RCC患者暴露在辅助免疫治疗的潜在毒副作用中会导致严重的过度治疗。因此,改进基于风险的选择、选择最有可能复发的患者,从而最有可能获得辅助免疫治疗的有利风险-效益比是至关重要的。
放射组学是一个不断发展的领域,可对从医学成像中提取的定量特征进行计算机化分析。在肿瘤学中,放射组学旨在发现图像中可能与癌症生物学有关的隐藏模式并提供预后信息。在RCC方面,由于分子异质性已被确定为一个重要的预后因素,因此可以假设,与肿瘤异质性相关的放射学特征可以提供有用的预后信息。以前的一些研究已经评估了利用放射组学来预测肾脏肿块患者的各种结果。然而,这些研究主要集中在预测恶性肿瘤的风险、组织学和肿瘤等级。

近日,发表在European Radiology杂志的一项研究明确了在既定的预后生物标志物的基础上增加从术前CT中提取的放射学特征是否能提高预测RCC患者手术切除后无病生存(DFS)的能力,并协助临床进一步筛选那些最有可能从辅助治疗中获益的患者。
本项回顾性研究包括453名接受肾切除术的非转移性RCC患者。使用术后生物标志物(年龄、分期、肿瘤大小和等级),并通过在术前CT上选择和不选择放射组学训练了Cox模型来预测无病生存(DFS)。使用C统计学、校准和决策曲线分析(重复十倍交叉验证)来评估模型。
在多变量分析中,四个选定的放射组学特征之一(wavelet-HHL_glcm_ClusterShade)对DFS有预后作用,调整后的危险比(HR)为0.44(p = 0. 02)、美国癌症联合委员会(AJCC)的阶段组(III级对I级,HR 2.90;p = 0.002)、4级(对1级,HR 8.90;p = 0.001),年龄(每10年HR 1.29;p = 0.03)和肿瘤大小(每厘米HR 1.13;p = 0.003)。临床-放射学联合模型的判别能力(C = 0.80)优于临床模型(C = 0.78;p < 0.001)。决策曲线分析显示,在用于辅助治疗决策时,联合模型有净收益。在5年内疾病复发的典型阈值概率≥25%的情况下,使用联合模型与临床模型相比,相当于多治疗了9名不治疗就会复发的患者(每1000人评估),而假阳性的预测没有增加。
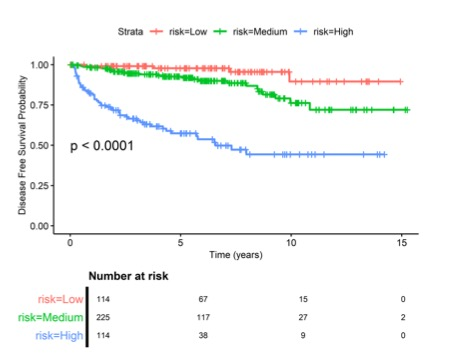
图 肾切除术后无病生存概率的Kaplan-Meier分析,根据放射学+临床模型的联合预测,疾病复发/死亡的低、中、高风险患者的生存概率。风险组由风险预测的四分位数定义
本项研究表明,将基于CT的放射组学特征添加到已建立的预后生物标志物中改善了术后复发风险的评估,有助于指导辅助治疗的决策。
原文出处:
Dominik Deniffel,Kristen McAlpine,Felix N Harder,et al.Predicting the recurrence risk of renal cell carcinoma after nephrectomy: potential role of CT-radiomics for adjuvant treatment decisions.DOI:10.1007/s00330-023-09551-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肾细胞癌# #放射组学#
28
学习了,受益良多。
24
不错,学习了。
20
不错,学习了。
25
不错,学习了。
21