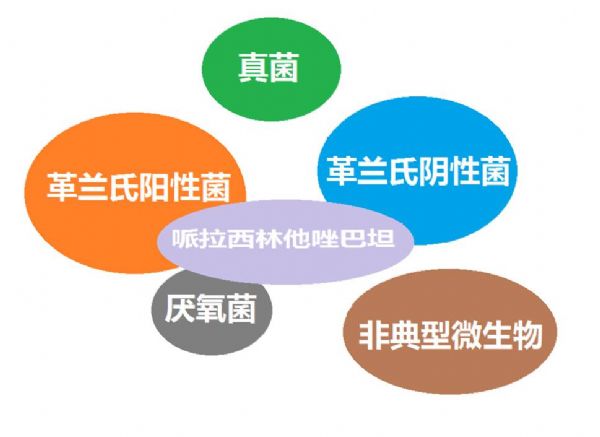
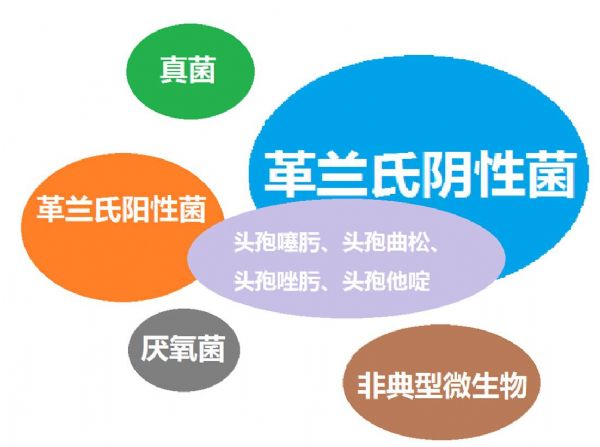
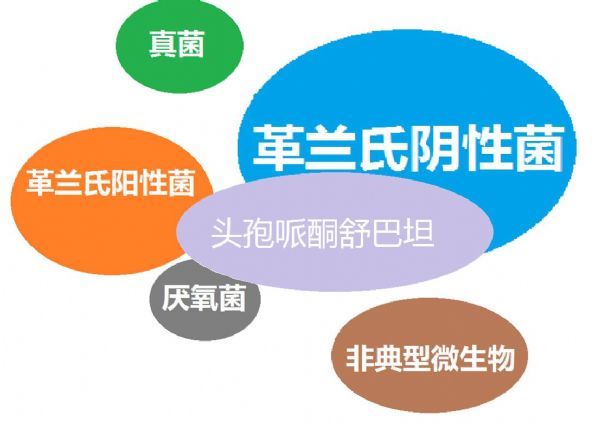
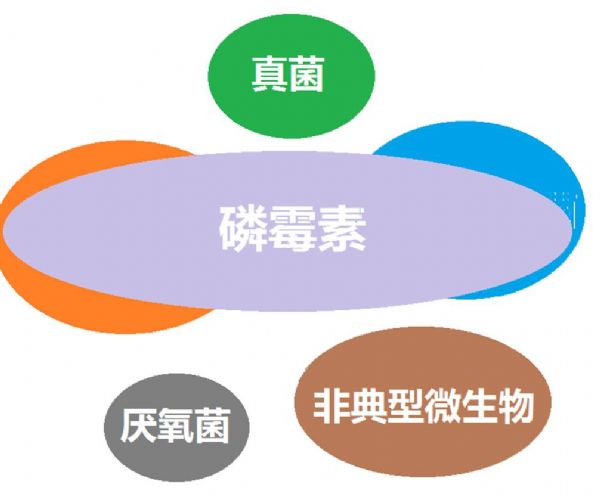
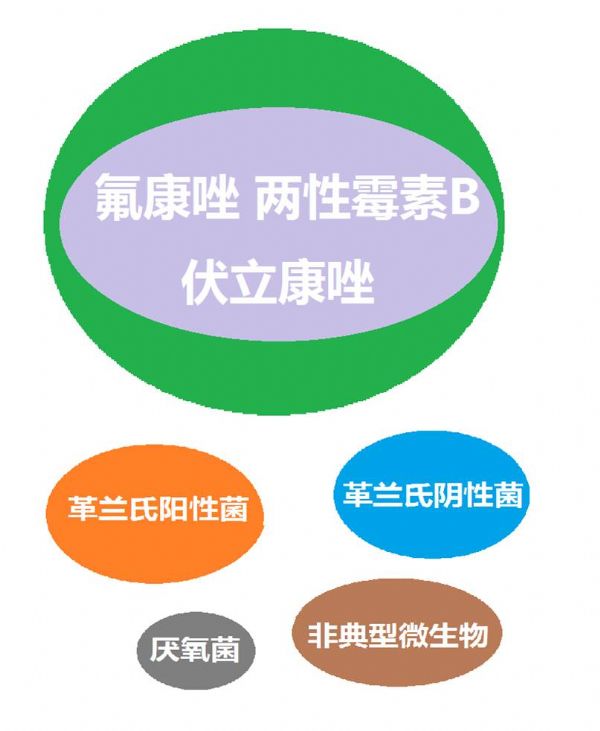
看图“话”抗菌谱,赶紧收藏!
2018-02-05 周雪松 医学界呼吸频道
在临床工作中药物抗菌谱容易记混,有些药物抗菌谱不清楚,那么我们今天来看图“话”抗菌谱,把抗菌谱“画”清楚,“话”明白。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






























学习了谢谢分享!!
70
学习了谢谢分享!!
80
很棒~
63
#抗菌#
28
谢谢分享
65
#抗菌谱#
22
学习学习学习
68
学习了谢谢了
25
学习
19
学习了谢谢分享!!
27