Neurology:神经元异常迁移和迁移后发育导致的癫痫和皮质畸形的长期结果
2022-07-08 MedSci原创 MedSci原创
癫痫和MCD患者在发病后20年内的缓解率为38%。MCD的单侧分布与实现缓解的3倍概率有关。
大脑皮层含有兴奋性中间神经元和抑制性中间神经元。兴奋性中间神经元是局部产生的,并通过径向滑行迁移到大脑皮层内的最终位置。抑制性中间神经元是在大脑皮层的较远区域产生的,通过跳跃性移动沿着切向路径进行迁移。近期,发表在NEUROLOGY杂志上的研究评价了癫痫和皮质发育畸形(MCD)患者的长期结果。

研究人员对因神经元迁移和迁移后组织受损的癫痫和MCD患者进行了历史队列研究,随访期≥5年。对于每个患者,在神经放射学专家进行准确的神经影像学重新评估后,对MCD进行了分类。主要结果是癫痫缓解,定义为无癫痫发作≥5年。使用Kaplan-Meier估计值进行生存分析,并进行单变量和多变量Cox回归分析,以评估基线变量与缓解相关的可能因素。
结果显示,该队列包括71名患者(男/女31/40),随访时间中位数为17年(1506人·年)。癫痫发作时的平均年龄为12.4±7.2岁。30.4%和40.9%的患者有智力障碍和神经系统缺陷。超过60%的患者为难治性癫痫。在3名接受癫痫手术的患者中,MCD的诊断被组织学所证实。
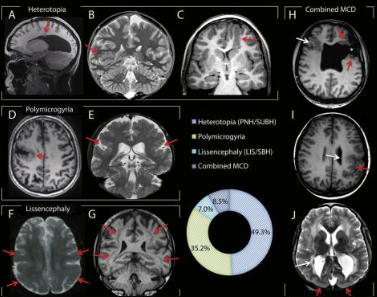
在最后一次就诊时,44%的患者在过去一年中没有发作,但他们都没有停止抗癫痫药物治疗。30名患者在其疾病史的某个阶段实现了缓解(42.2%),而41人(57.8%)在≥5年内从未缓解过。在纳入后的20年里,累积缓解率为38%。在Cox模型中,MCD的单侧分布(HR=2.68,95%CI 1.04-6.92)和发病时的低发作频率(HR=5.01,95%CI 1.12-22.5)与缓解显著相关。
综上,癫痫和MCD患者在发病后20年内的缓解率为38%。MCD的单侧分布与实现缓解的3倍概率有关。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
65
#长期结果#
67
#迁移#
58
学习了,谢谢分享
68
#发育#
54
#畸形#
66