Lancet Neurol:Ganaxolone治疗CDKL5缺乏症的疗效
2022-05-11 Nebula MedSci原创
Ganaxolone能显著降低CCD相关癫痫发作的频率
CDKL5缺乏症 (CDD) 是一种罕见的、X染色体相关的发育性癫痫性脑病,其特征是严重的整体发育障碍和癫痫发作,可在出生后的头几个月发病,目前仍难以治疗。
Ganaxolone(加奈索酮),一种实验性的神经活性类固醇,在一项涵盖CDD患者的开放标签的2期临床试验中降低了癫痫发作频率。
今年3月,基于Marigold研究结果,Ganaxolone获得FDA批准2岁及以上的CCD患者。Ganaxolone是首个获得批专门用于治疗CDD的药物。
Marigold研究是一项在8个国家的39个诊所开展的双盲、安慰剂为对照的3期试验,招募了2-21岁的携带CDKL5致病或可能致病性变异的、28天至少发生16次严重的运动痉挛的患者。受试患者(1:1)随机接受Ganaxolone或安慰剂治疗17周。主要疗效终点是第17周时主要运动痉挛发作频率的变化。
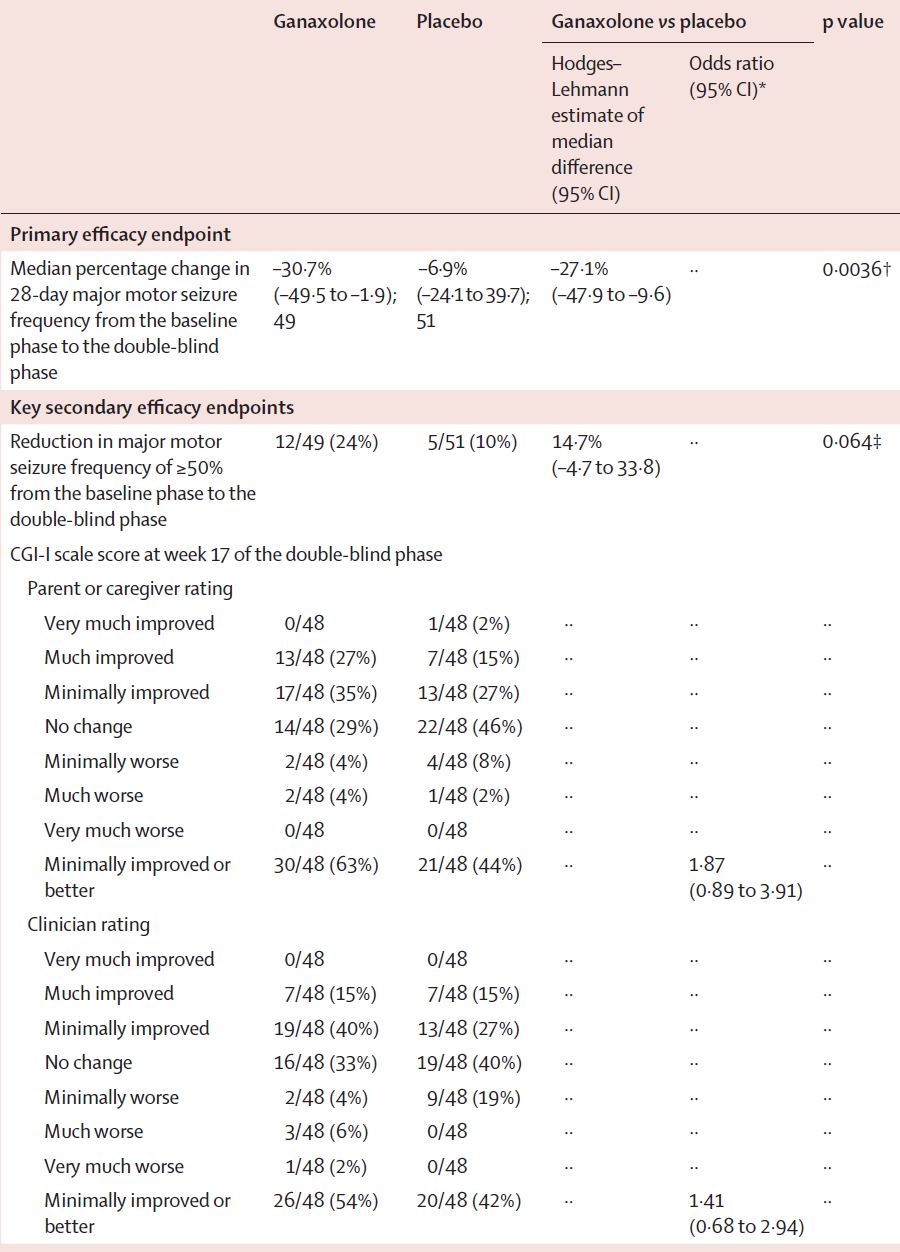
两组主要运动痉挛频率的变化
2018年6月25日-2020年7月2日,共筛查了114位患者,其中101位(中位年龄 6岁)被随机分至Ganaxolone组(n=50)或安慰剂组(n=51)。所有患者至少接受了一剂研究药物,但因Ganaxolone组有一位患者无基线癫痫发作频率被排除主要分析。Ganaxolone组和安慰剂组的28天主要运动痉挛的发作频率变化比例分别是-30.7%和-6.9%(p=0.0036)。Hodges-Lehmann估计的对Ganaxolone和安慰剂反应的中位差值为-27.1%。
两组的主要疗效和部分次要疗效结果
Ganaxolone组和安慰剂组分别有43位(86%)和45位(88%)患者发生了需干预的不良反应事件。Ganaxolone组发生于≥10%的患者的不良反应有嗜睡、发热和上呼吸道感染,发生率均高于安慰剂组。Ganaxolone组有6位(12%)患者发生了严重不良反应,安慰剂组有5位(10%)。Ganaxolone组和安慰剂组分别有2位(4%)和4位(8%)患者中断试验,无死亡病例。
总之,与安慰剂相比,Ganaxolone能显著降低CCD相关癫痫发作的频率,且耐受性良好。
原始出处:
Elia M Pestana Knight, et al. Safety and efficacy of ganaxolone in patients with CDKL5 deficiency disorder: results from the double-blind phase of a randomised, placebo-controlled, phase 3 trial. The Lancet Neurology. May, 2022. https://doi.org/10.1016/S1474-4422(22)00077-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ANA#
51
#Neurol#
0
#Lancet#
46
#CDK#
55
lancet上果然牛,感谢梅斯更新及时
54