混杂因素控制策略—随机、限制、配对、分层、回归和工具变量法
2016-06-16 MedSci MedSci原创
临床研究的发展可以说是与混杂因素和偏倚的“斗争”密不可分的。临床研究发展到现在,也有很多方法控制混杂因素。混杂控制的水平直接影响到研究的质量!MedSci小编这里把常见的控制混杂的策略全部告诉大家了哦! 随机化 研究对象随机分配于各组,以使比较组之间在混杂因素的分布上达到均衡,常用于实验性研究,以临床实验中多见。可针对已知或未知混杂,但是当样本量较小时,由于机会的原因,可能并不能完全平衡两
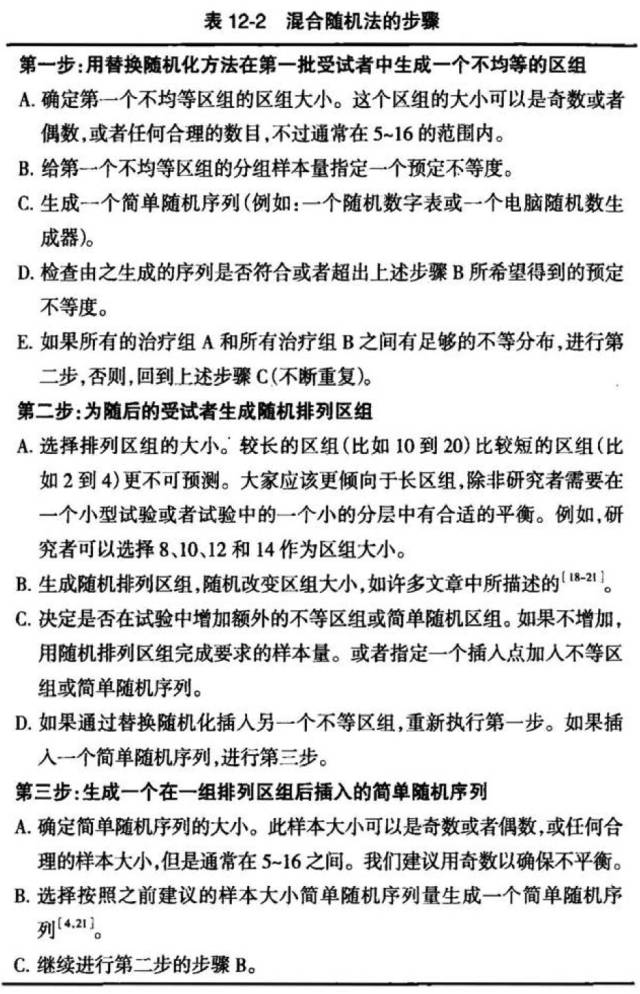
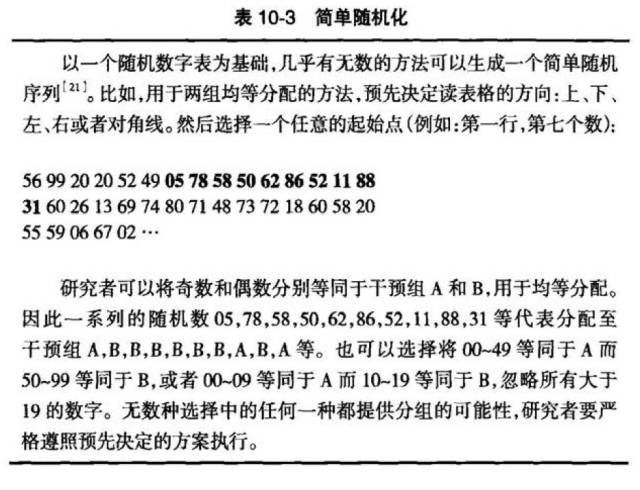
临床研究的发展可以说是与混杂因素和偏倚的“斗争”密不可分的。临床研究发展到现在,也有很多方法控制混杂因素。混杂控制的水平直接影响到研究的质量!MedSci小编这里把常见的控制混杂的策略全部告诉大家了哦! 随机化 研究对象随机分配于各组,以使比较组之间在混杂因素的分布上达到均衡,常用于实验性研究,以临床实验中多见。可针对已知或未知混杂,但是当样本量较小时,由于机会的原因,可能并不能完全平衡两组之间的混杂因素,样本量越大,这一问题越小。 RCT在进行分组时,采用完全随机的方法,也就是说每个病例进入病例组和对照组的概率是相同的,这样看得见的和看不见的混杂因素在各组的分布都是均衡的。如果RCT实施过程严格执行随机方案,可以认为只有干预因素在组间是不同的。当然,这仅仅是理论上的。在实际上,RCT时还要考虑分层,区组,以及中心化等一些策略,让随机更有效。 限制 针对某些可能的混杂因素,对研究对象的入选条件加以限制。限制使混杂因素恒定,没有变异,消除了暴露-混杂,疾病-混杂的联系。优点在于概念易懂,然而缺点是符合条件的研究对象减少;筛检大量个体,只能入选其中一部分,这样效率太低;影响结果外推;限制范
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











收藏了。
73
收藏学习
69
好好
71
学习了,统计好难
65
说得很细
117
先收藏了
42
先收藏,再学习
81